Xcode Life's Genetic Osteoarthritis DNA Report
Researchers have identified several genes associated with osteoarthritis.
In the sample report below, we've attempted to analyze some important genes that increase the risk of osteoarthritis.
You can identify your genetic risk of osteoarthritis by using your 23andMe DNA data and placing an order for the Gene Health Report.
What is Osteoarthritis?
Osteoarthritis (OA) is a degenerative disease of the joints. The condition makes joints stiff, weak, and painful and reduces mobility.
This is very common in older adults, and OA can affect all body parts, including knees, hands, shoulders, and hips.
Causes Of Osteoarthritis
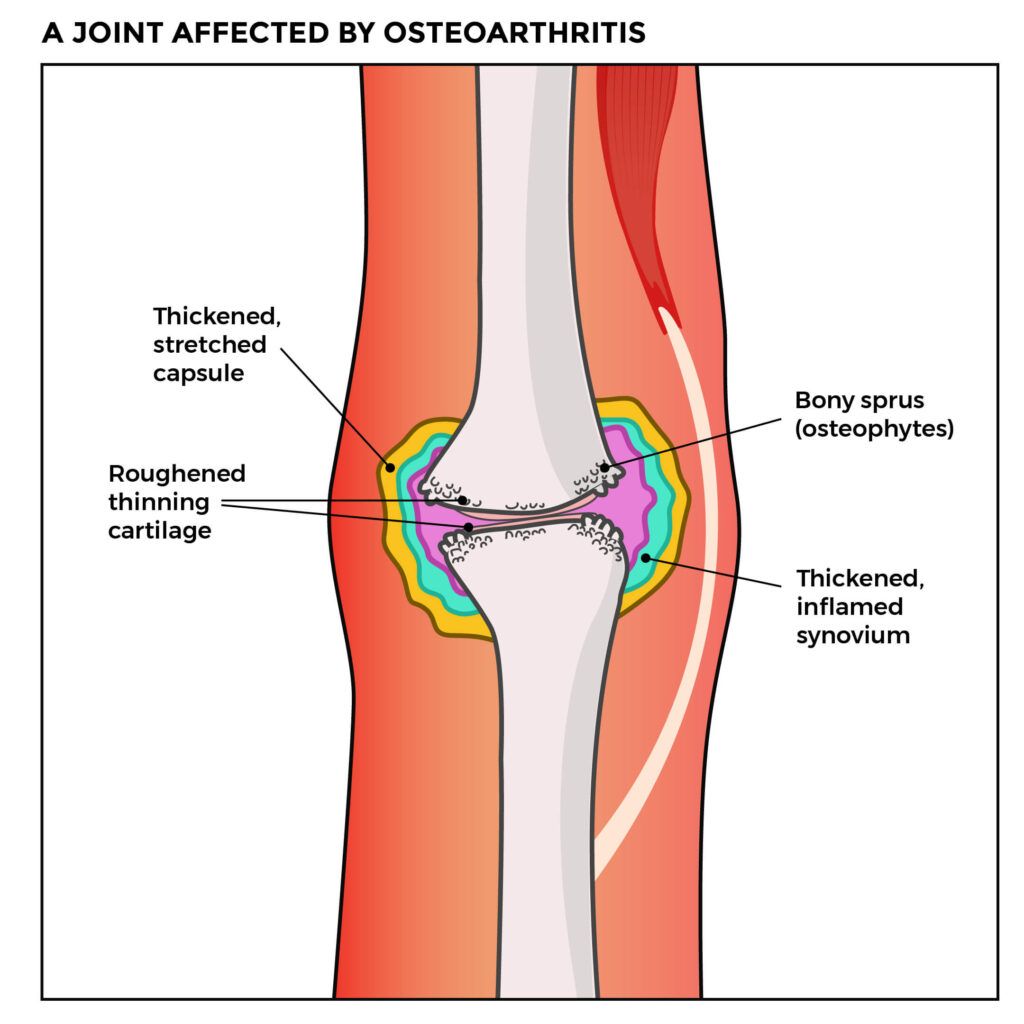
Cartilage is a flexible tissue that covers joints and bones.
It allows joints to move smoothly without friction.
OA breaks down the cartilage, so the joints and bones start rubbing against one another as they move. This leads to pain, swelling, stiffness, and lowered mobility.
OA is a wear and tear condition.
As people age, the cartilage and joints go through age-related wear and tear, causing pain and stiffness.
Studies show that up to 35-65% of cases of osteoarthritis could be genetically influenced. We will discuss more on the genetic influences in the coming sections.
There could be so many environmental and lifestyle causes that increase a person’s risk of developing OA.
Symptoms Of Osteoarthritis
Some of the commonly experienced symptoms of OA are
- Pain during movement
- Stiffness in the joints and inability to move (after a period of inactivity or in the mornings)
- Tenderness in the joints when pressure is applied
- A grinding or grating sound when you move the joints
- Inability to move joints completely, in its full motion range
Source: https://www.versusarthritis.org/about-arthritis/conditions/osteoarthritis/
Is Osteoarthritis Genetic?
Studies show that OA has a polygenic inheritance.
This means that the condition is influenced by multiple genes instead of just one.
The age of onset of OA, its progression, and the severity of the condition could all be influenced by different gene changes and their interactions.
OA in the hands and hips could be 65% inherited, while OA in the knee could be about 40% inherited.
Are Specific Genes Linked To Osteoarthritis?
As mentioned above, multiple genes determine a person’s risk of developing OA. Some of the important ones are mentioned below.
Collagen genes
The COL2A1 gene provides instructions for producing type II collagen. This collagen makes connective tissues like cartilage stronger and gives them flexibility.
Changes in this gene may lead to a lowered production of type II collagen, leading to early cartilage breakdown and OA.
Other genes that control the production of collagen in the body may also increase or decrease a person’s risk of developing OA. These include
| Genes | Manifestation |
| COL11A1 | Early onset of OA |
| COL11A2 | Early onset of OA |
| COL1A1 | Protective against hip OA in females and people assigned female at birth |
| COL9A1 | Early onset of knee OA |
Interleukin genes
Interleukins are types of proteins that are produced by White Blood Cells (WBCs).
These play a role in cell-cell communication.
Certain genes that control the production of interleukins may increase or decrease a person’s risk of developing OA.
Some of these interleukin genes are:
| Genes | Manifestation |
| IL-1A, IL-1B, IL1RN | Can cause knee and hip OA |
| IL4R | Can cause hip OA in females and in people assigned female at birth |
| IL6R | Can cause hip OA |
| IL17A, IL17F | Increases risk of developing OA |
Other genes that have been associated with OA are:
| Genes | Manifestation |
| Insulin-like growth factor 1 (IGF-1) | Increases risk of developing OA |
| Matrilin-3 (MATN3) | Can cause early onset of OA in hands and knees |
| Vitamin D receptor (VDR) | Increases overall risk of developing OA |
| Cartilage Oligomeric Matrix Protein (COMP) | Early onset of hip OA |
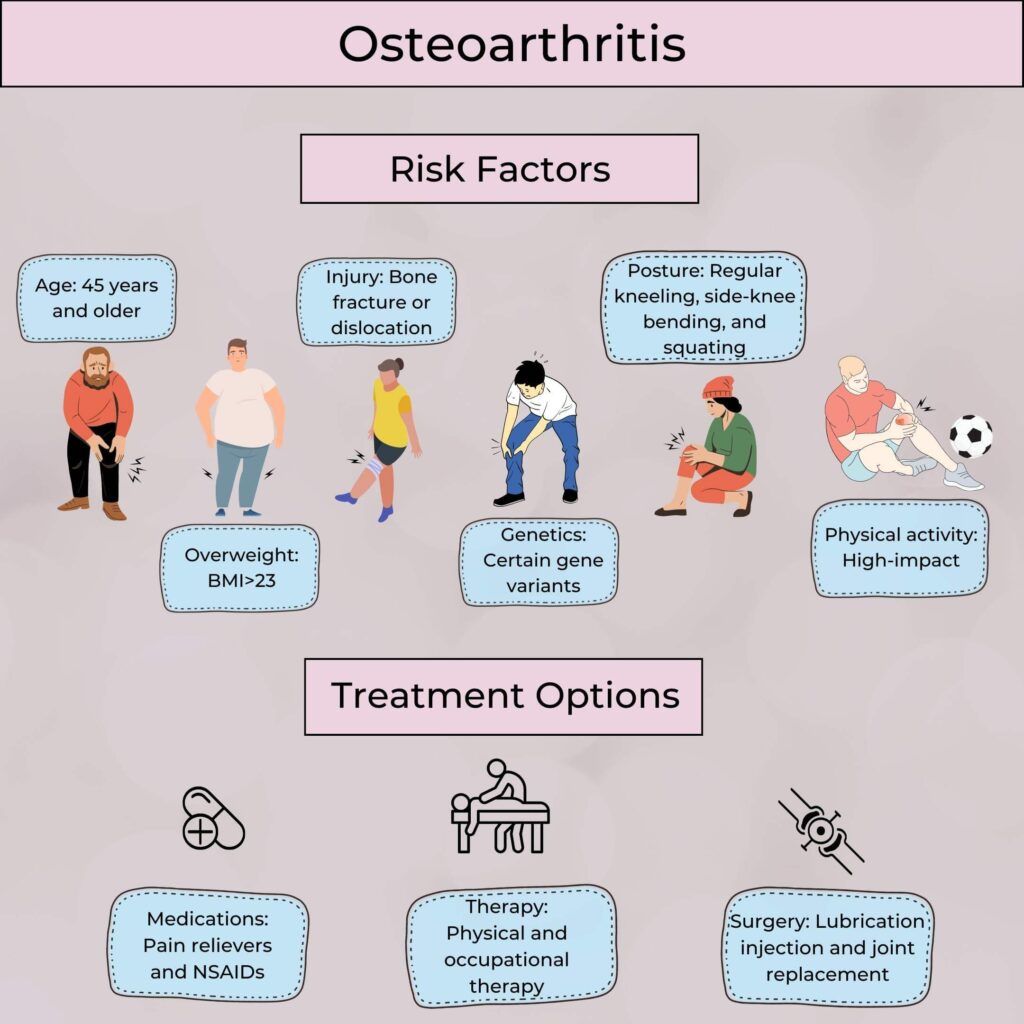
Other Risk Factors For Osteoarthritis
Some of the non-genetic risk factors for developing osteoarthritis are:
Age
Since OA is a wear and tear disease, the risk of developing the condition increases with age.
Gender
OA occurs more frequently in women and people assigned female at birth than men and people assigned male at birth.
BMI Levels
Carrying excess weight puts unnecessary stress on the joints, leading to OA.
Injuries In The Joints
Any serious injury to the joints that didn’t heal well may increase a person’s risk of developing OA.
Congenital Deformities
Any deformity to joints that happened by birth may increase the person’s risk of developing OA.
Congenital deformities are one of the most common reasons people develop OA in the hip.
Vitamin D Deficiency
When the cartilage gets broken down, the body tries to repair the same using Vitamin D. Lack of vitamin D may prevent the body from healing the cartilage and lead to OA.
Image: Risk factors and treatment for osteoarthritis
Summary: Is Osteoarthritis Genetic?
While osteoarthritis could result from certain medical conditions, age, and injuries, genetics remains an important cause.
Genetics may influence the age of onset, the progression, and the severity of symptoms of OA.
Genetic testing can help understand your risk of developing the condition. If you have close family members with OA, then genetic testing may help.
Preventive medications, physical activities, and other lifestyle changes can bring down the damage to the cartilage and delay the onset of OA in high-risk individuals.