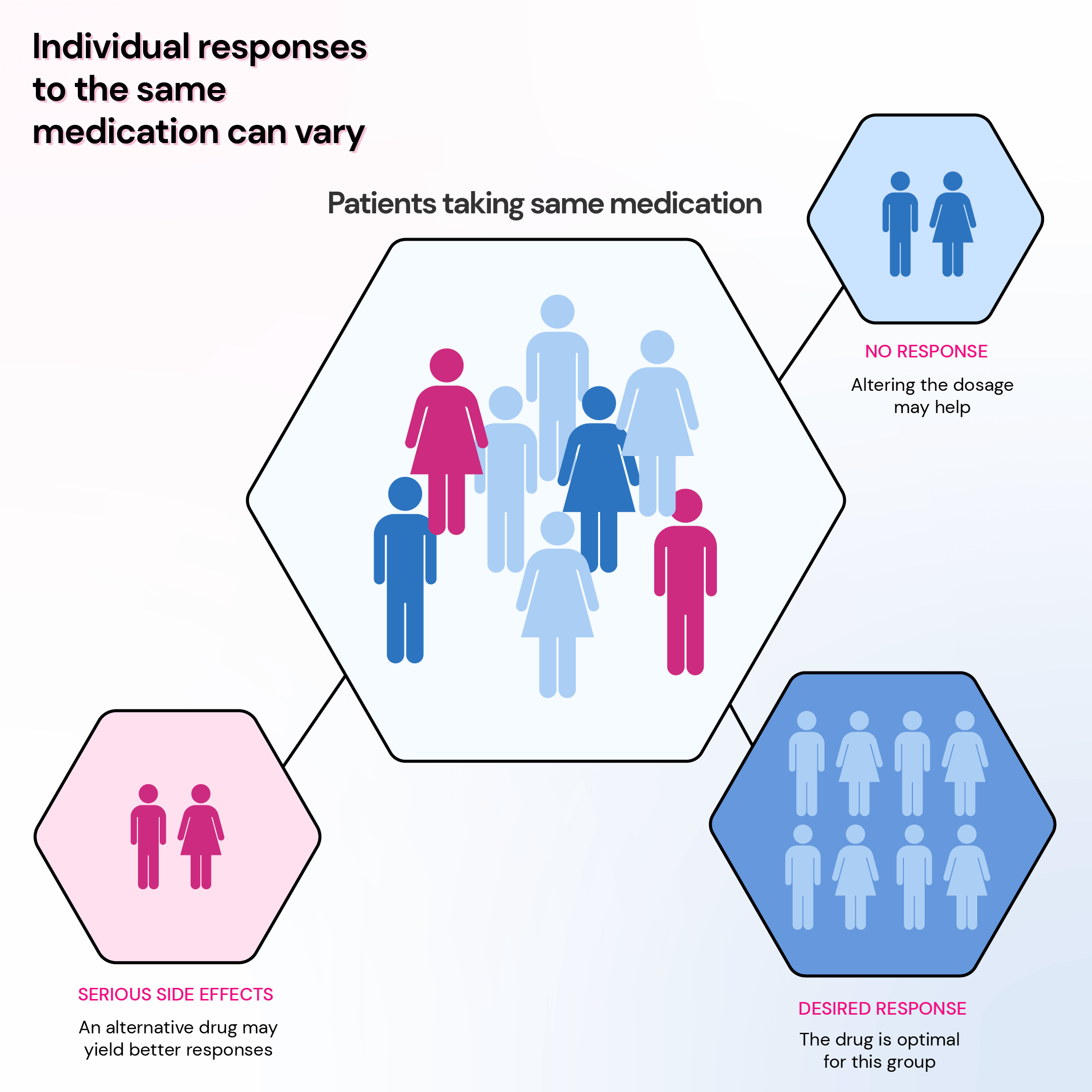
Last year, my cousin and I were prescribed the same antibiotic for similar infections. While I recovered quickly, she experienced severe side effects, leading us to question why. This personal experience brings us to the concept of pharmacogenomic testing – a revolutionary method that uses an individual’s genetic profile to predict drug response. Intriguingly, it reveals why medications don't have a uniform effect on everyone. However, pharmacogenomic testing isn't universally applicable. Understanding its scope and limitations is vital for those considering it. This article delves into the heart of why this groundbreaking testing, while transformative for some, remains out of reach or ineffective for others. We'll uncover the challenges and limitations surrounding pharmacogenomic testing and urge you to engage with this pivotal topic. Our collective understanding and advocacy can pave the way for more inclusive and effective healthcare solutions.
Did You Know?
While some genes may affect the drug's efficacy, others may result in nasty side effects. That is why we want to help you and your physician understand your genetic changes to optimize treatment and outcomes. Xcode Life's Personalized Medicine Report profiles gene variants that influence your metabolic response to various drug therapies. The results of this report can be used as a supplement to the clinical decision-making process and reduce the cost and time associated with a trial-and-error treatment.
You can get your report using your existing DNA raw data file. No new DNA test required! Learn More
What Is Pharmacogenomics?
Pharmacogenomics is founded on the principle that genetic variations (single-letter changes in DNA that make everyone their unique self) among individuals influence their drug metabolism, transport, and response.
These genetic variations can impact an individual's drug effectiveness, safety, and dosage requirements.
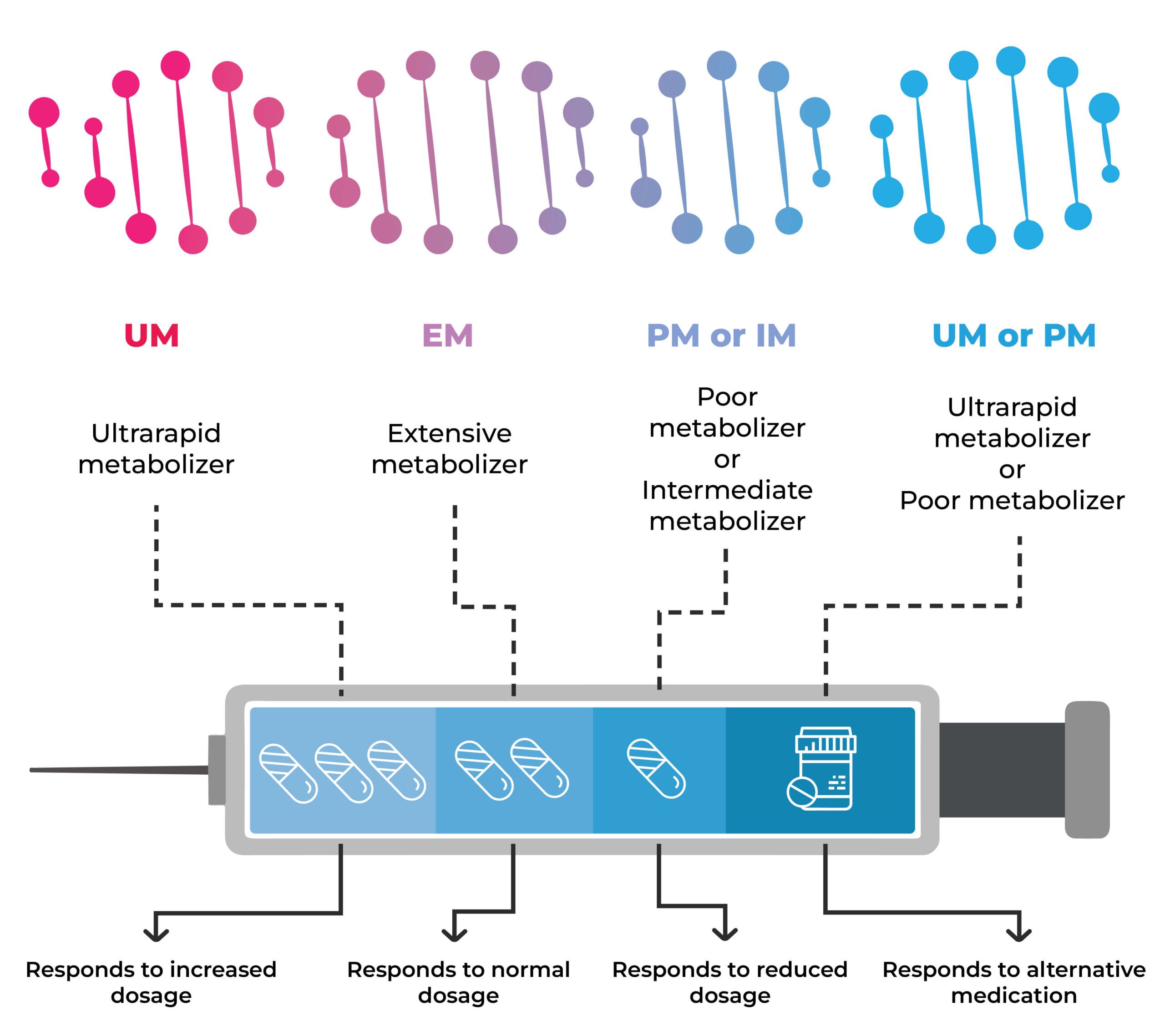
For instance, some individuals possess genes that accelerate drug breakdown. Consequently, they may require a higher dosage to achieve the desired therapeutic effect than those who metabolize the drug more slowly.
Conversely, some individuals have genes that slow down drug metabolism. A lower dosage may be necessary to prevent adverse side effects.
Furthermore, a person's genetic makeup can affect their susceptibility to adverse reactions from certain medications, such as allergic responses, bleeding complications, or liver problems.
How Does Pharmacogenomics Work?
Pharmacogenomics utilizes pharmacogenetic tests to analyze an individual's DNA and identify variations in genes known to influence drug response.
These genetic factors play a pivotal role in several key aspects of the drug interaction process, including:
- Drug receptors
- Genes determine the type and quantity of receptors on the surface of cells that drugs need to attach to for maximum functioning.
- For example, in breast cancer, the drug T-DM1 targets the HER2 receptor on cancerous cells. A pharmacogenetic test helps determine if T-DM1 is the right treatment based on the amount of HER2 protein in the tumor.
- Drug uptake
- Genetic factors influence the active uptake of certain drugs into tissues and cells, affecting their efficacy.
- For example, in the context of statins and muscle problems, the SLCO1B1 gene influences the transport of statins into the liver. Genetic testing helps determine the best statin or dosage to prevent complications.
- Drug breakdown
- Genetic variations impact the rate at which the body breaks down drugs, influencing the required dosage.
- For example, regarding depression and amitriptyline, genes like CYP2D6 and CYP2C19 influence the breakdown of the drug. Pharmacogenetic tests assist in prescribing the right dose or an alternative medication based on the breakdown speed.
- Targeted drug development:
- Pharmacogenomic approaches target the root cause of diseases by addressing specific genetic mutations rather than just treating symptoms.
- For example, in cystic fibrosis and ivacaftor, the drug addresses mutations in the CFTR gene by targeting the dysfunctional channel. This approach is customized to specific genetic mutations, ensuring effectiveness.
What Is Pharmacogenomic Testing?
Pharmacogenomic testing, or pharmacogenetics, is a lab test typically done using saliva, blood, or cheek cell samples.
This testing is part of precision medicine, which integrates genetic, environmental, and lifestyle data to develop personalized disease treatment and prevention approaches.
Pharmacogenomic testing can serve various purposes, such as:
- Predicting the likelihood of efficacy or toxicity of a drug before prescribing it.
- Adjusting the drug dosage based on the patient's genetic profile.
- Identifying the most suitable drug or drug combination for a patient.
- Monitoring the response and adverse effects of a drug during treatment.
- Preventing or managing drug-drug or drug-gene interactions.
Who Needs Pharmacogenomic Testing?
Pharmacogenomic testing might be suggested by your healthcare provider when initiating specific medications.
It is also considered if you are currently taking a drug that isn't giving the desired results or is causing severe side effects.
While not all medications have associated pharmacogenetic tests, some common examples include:
- Abacavir, utilized in HIV treatment
- Carbamazepine, prescribed for epilepsy
- Tamoxifen, employed in breast cancer treatment
- Warfarin and clopidogrel, medications used as blood thinners
Xcode Life's Pharmacogenomic Test covers more than 500 genetic variants for drug responses.
Pharmacogenomic Testing Results
What Can You Expect?
Upon getting your pharmacogenomic test results, you may receive these key information:
- Genotype information: Provide a detailed report of your genetic makeup, specifying the particular combination of genetic variations analyzed.
- Genotype implications for drug response: Summarizes how your genetic makeup will likely influence your response to certain medications.
- Guidance for medication management: Offers recommendations for optimizing your medication regimen and adjusting dosages based on your pharmacogenomic profile.
How To Interpret It?
Pharmacogenomic test results use a standardized nomenclature, ensuring consistent interpretation across different laboratories.
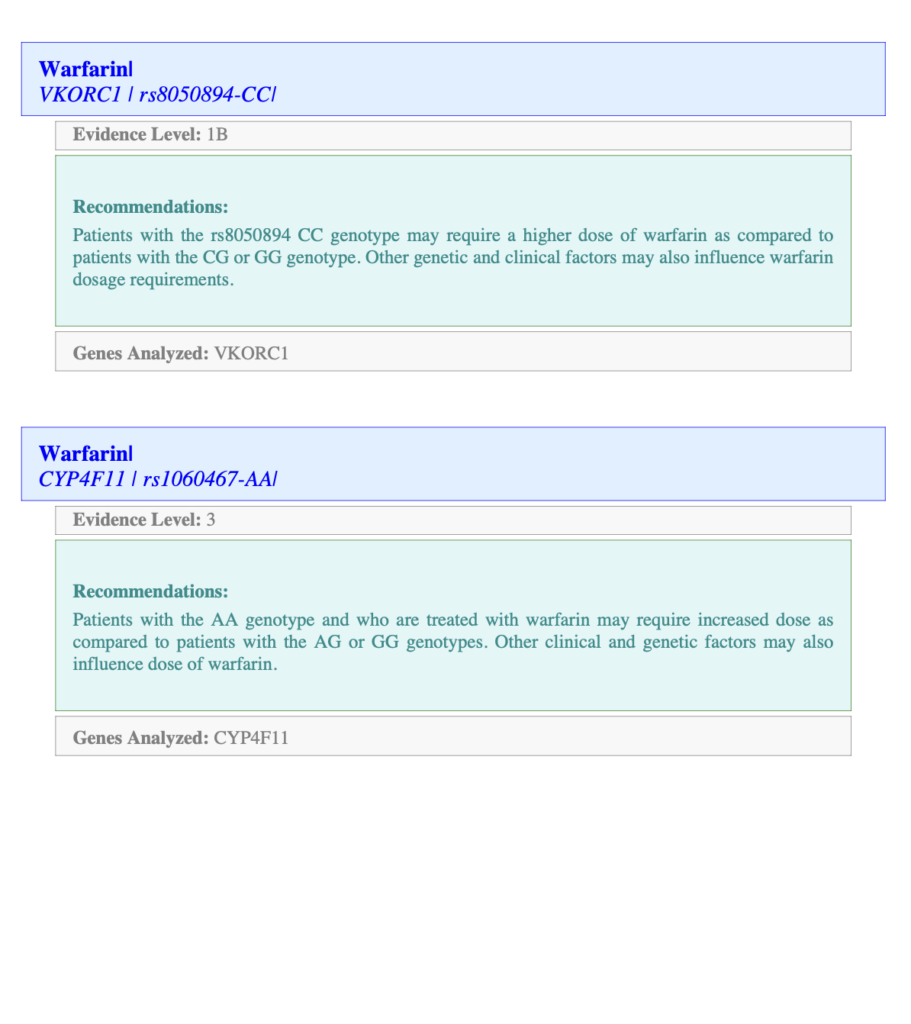
Xcode Life's report provides details on the genetic variant analyzed for each drug. In the image below, the first line after the drug name "Warfarin," you can see the gene and the variant analyzed, along with your genotype.
The Evidence Level stands for how strong the association is between the variant and the drug interaction. Level 1 is the strongest.
The Recommendations section provides information on the genotype in the context of drug interaction.
What’s The Accuracy?
While pharmacogenomic testing is generally accurate in predicting drug responses for most genes, accuracy can vary based on the gene and test type.
It's essential to know that pharmacogenomics is a developing field that requires ongoing research to understand the complex interplay between genes and drug responses fully.
What Are The Current Applications
Pharmacogenomics has been applied to several areas of medicine, such as psychiatry, cardiology, oncology, neurology, and infectious diseases.
Some examples of drugs that have pharmacogenetic guidelines or labels include:
- Warfarin: This blood thinner needs careful monitoring and dose adjustment based on your genes (CYP2C9 and VKORC1) and your metabolizer status
- Clopidogrel: If your CYP2C19 gene isn't very active (slow metabolizer), this antiplatelet drug might not work well for you.
- Abacavir: For this antiretroviral drug, having the HLA-B*5701 gene may lead to severe hypersensitivity reactions.
- Tamoxifen: If your CYP2D6 gene is not very active, this anticancer drug might not work as effectively.
- Codeine: Your CYP2D6 gene activity matters for this painkiller. High (fast metabolizer) or low (slow metabolizer) activity can lead to overdose or not enough pain relief.
What Are The Current Limitations
Pharmacogenomics' limitations include a variety of factors that go beyond genetic makeup and can impact the effectiveness of personalized drug therapy.
Some key limitations include:
- Incomplete genetic explanation: While genetics play a crucial role in determining drug response, it needs to provide a comprehensive understanding of how the body processes medications. Other factors, such as environmental influences, epigenetics, and post-translational modifications, contribute to the overall drug response.
- Interactions with other medications: The effectiveness of pharmacogenomic-guided treatments may be influenced by concurrent medications. The interactions between different drugs can affect their metabolism and alter the expected therapeutic outcomes.
- Impact of health conditions: Certain conditions can significantly influence the metabolism and medication response. Pharmacogenomic information may not fully capture the complexity of these interactions, leading to challenges in accurately predicting drug efficacy and safety.
- Lifestyle factors: Lifestyle choices, such as diet, exercise, tobacco, and alcohol use, can affect medication processing within the body. These factors are not always considered in pharmacogenomic testing, making it challenging to predict drug responses accurately.
- Cost of testing: Pharmacogenomic testing can still be expensive despite lowering costs. This cost factor could limit the widespread adoption of pharmacogenomics in clinical practice.
- Complex data interpretation: Interpreting pharmacogenomic data requires specialized knowledge and expertise. Healthcare providers may struggle to interpret genetic information accurately, leading to wrong treatment decisions.
Should I Get A Pharmacogenomic Test?
After discussing it with your doctor and carefully considering its potential benefits and drawbacks, the decision to undergo a pharmacogenomic test should be made.
It would help if you considered the following questions:
- Do you have a medical condition that requires or might benefit from pharmacogenomic testing?
- Is there a family history of adverse drug reactions or unsatisfactory treatment outcomes linked to pharmacogenomics?
- Can you access a reliable, accredited laboratory that performs pharmacogenomic testing?
- Have you acquired enough information and understanding regarding pharmacogenomics and its implications for your health?
- Are you guided and supported by a qualified professional capable of interpreting and applying the outcomes of pharmacogenomic testing?
Remember, the benefits of pharmacogenomic testing vary from person to person, as it personalizes medication management based on individual genetic characteristics.
It's important to consult your doctor to determine if pharmacogenomic testing is appropriate for you.
Summary
Pharmacogenomics aims for personalized drug therapy, exploring how genes influence how our bodies respond to medications.
Results provide genotype details, drug response implications, and medication management guidance. However, accuracy varies by gene and test type.
Pharmacogenomics has applications in various medical fields. Despite this, limitations exist, including incomplete genetic explanation, drug interactions, health conditions, lifestyle factors, cost, and complex data interpretation.
Whether to get a pharmacogenomic test depends on factors like medical conditions, family history, access to testing, and guidance from a qualified healthcare professional.
Pharmacogenomic testing isn't a magic fix; decisions should involve consulting your doctor and carefully considering the pros and cons.
References
https://medlineplus.gov/genetics/understanding/genomicresearch/pharmacogenomics/
https://medlineplus.gov/lab-tests/pharmacogenetic-tests/
https://www.cdc.gov/genomics/disease/pharma.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4000170/
https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling
https://clinicalinfo.hiv.gov/en/glossary/hla-b5701-test
https://my.clevelandclinic.org/health/articles/pharmacogenomics




