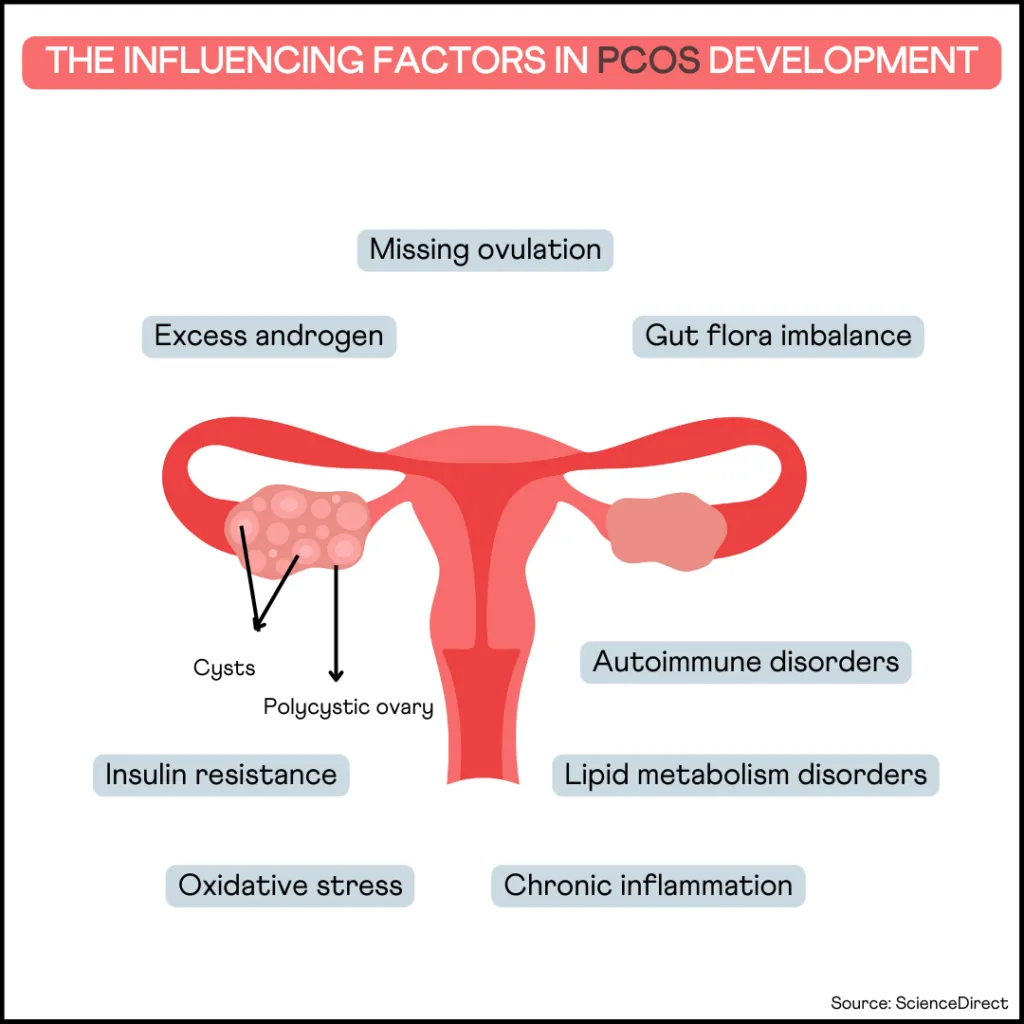
Polycystic ovarian syndrome (PCOS) is the most prevalent hormonal disorder affecting females. It is a common cause of menstrual irregularities and infertility during reproductive age. It causes symptoms affecting various body parts, from the skin to the hair. Emerging research suggests an association between PCOS and autoimmune disorders; This raises an important question: Is PCOS an Autoimmune Disease?
Check your DNA raw data for gene variants related to PCOS
What is Polycystic Ovarian Syndrome (PCOS)?
PCOS is a common hormonal disorder that can affect women of reproductive age.
The condition is caused by an imbalance of hormones, which can lead to irregular periods, excess hair growth, and difficulty getting pregnant.
The ovaries produce excessive male hormones (testosterone), which can cause the ovaries to become enlarged and develop cysts.
Although there is no cure for PCOS, treatment can help manage the symptoms.
Etiology of Autoimmune Diseases
Sometimes the immune system makes a mistake and attacks the body's tissues or organs. This is called autoimmunity.
Although the exact reason for autoimmunity is unknown, various mechanisms have been suggested for its development.
Sequestered antigens
Sequestered antigens are some proteins in the body that are hidden from cells of the immune system, and thus the immune system never encounters them.
When these proteins are released due to accidental trauma or injury, they can initiate an immune response that may trigger autoimmune diseases.
Molecular Mimicry
Molecular mimicry is one of the leading mechanisms by which infectious or chemical agents may induce autoimmunity.
Here, autoimmunity occurs due to the close similarity between environmental substances and certain components in the body.
When the immune system generates a response against these foreign substances, it cross-reacts with the body's tissue.
Drug-induced Protein Alteration
In some cases, drugs can bind to normal proteins and change their properties, making them targets for immune attacks.
Dysfunction of Tregs
Tregs or regulatory T cells are important in suppressing unnecessary immune reactions and maintaining homeostasis.
Failure or decrease of Tregs can cause autoimmune disease.
Is PCOS An Autoimmune Disease?
Although research doesn’t conclusively state that PCOS is an autoimmune disorder, studies point out many similarities between both.
Autoantibodies
Both in PCOS and autoimmune diseases, autoantibodies can be detected.
In fact, autoantibodies are the hallmark of the latter.
Some common autoantibodies seen in both conditions are antinuclear antibodies, anti-thyroid antibodies, and anti-islet antibodies.
Insulin resistance
Insulin resistance is a significant risk factor for PCOS and is seen in several autoimmune disorders, such as rheumatoid arthritis and systemic lupus erythematosus (SLE).
The hormone insulin regulates blood sugar levels by storing excess sugar as fat.
With insulin resistance, the cells stop responding to the hormone insulin; as a result, more and more insulin is secreted.
In PCOS, excess insulin causes hormonal fluctuations and disrupts ovulation.
In autoimmune diseases, increased inflammation may drive insulin resistance.
There’s not too much clarity on what causes insulin resistance in PCOS, but an underlying autoimmune reaction could be the cause in some people.
Systemic Inflammation
Inflammation is the first line of defense against infection and is crucial for injury healing.
Scientific evidence suggests that irregular inflammatory responses can underlie autoimmune diseases like inflammatory bowel disease and rheumatoid arthritis.
Studies have shown that women with PCOS are more likely to have low-grade systemic inflammation.
Hormonal Imbalance in PCOS and Autoimmune Disorders
Women with PCOS tend to have low levels of progesterone.
Progesterone is a hormone that occurs naturally in the body. It's involved in pregnancy and is produced mainly in the ovaries.
Progesterone is stimulated after ovulation.
Many people with PCOS have ovulation issues and therefore have lower progesterone levels.
With lower progesterone levels, estrogen is “unopposed,” leading to its excess levels in the body.
Increased estrogen production can trigger the secretion of autoantibodies.
Further, excess estrogen has also been tied to increased production of several proteins associated with inflammation like IL-4, IL-1, IL-6, and interferon-γ.
These effects are seen even after menopause.
Bottomline
Even with all these similarities, there’s no conclusive evidence to prove that PCOS is an autoimmune disorder.
Therefore, it still comes under the classification of endocrine (or hormonal) disorder.
Having said that, whether you have PCOS or autoimmune disorder, working on your immune system, lowering inflammation, and building up insulin sensitivity work well to manage the symptoms.
Avenues of Future Research and Conclusion
The presence of varying levels of autoantibodies in people with PCOS blows open a new avenue of research at a molecular level.
Since autoantibodies seem to affect long-term clinical management of PCOS, this new chapter of research can help discover better treatment options for those with PCOS.
Additional studies need to be performed at a genetic level to understand the contribution of autoimmunity to PCOS.
Summary: Is PCOS An Autoimmune Disease?
- PCOS is a common hormonal disorder that results in irregular menstruation and issues with fertility.
- Autoimmune disease occurs when your immune system misrecognizes your body’s cells as foreign and starts attacking them.
- Due to the presence of autoantibodies, insulin resistance, and low-grade inflammation in both conditions, PCOS is hypothesized to be an autoimmune disorder.
- The lower levels of progesterone and higher levels of estrogen found in people with PCOS seem to trigger autoimmunity.
- However, to date, there’s no conclusive evidence to prove that PCOS is an autoimmune disorder, nor is there any clarity on the contribution of autoimmunity to PCOS. Therefore, PCOS, by and large, remains an endocrine disorder.
References
- http://www.pathwaymedicine.org/autoimmune-disease
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3945069/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6421792/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3245829/
- https://pubmed.ncbi.nlm.nih.gov/9195137
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4871972/