It was long assumed that genes that contribute to irritable bowel syndrome (IBS) affect the gut and bowel. However, research reveals that most of the genes appear to have roles in the brain and the nerves that supply the gut. Considering these genetic influences, is it possible that IBS has a hereditary component to it? This article discusses both the genetic and environmental contributors to IBS, aiming to provide a clearer understanding of its potential hereditary nature and its impact on your health.
Overview Of IBS
IBS is a well-known condition affecting the digestive system, particularly the stomach and intestines.
It causes abdominal discomfort, such as cramps, pain, bloating, gas, and irregular bowel motions. The intensity differs from person to person.
IBS is chronic, which means it lasts for an extended period of time. While it might be annoying, most people with IBS do not have severe symptoms.
Managing food, lifestyle, and stress can often successfully control symptoms. In some circumstances, medication and treatment may be necessary.
IBS doesn't damage your gut or raise your risk of colon cancer. The focus is on managing symptoms and living well through self-care and medical help.
Is IBS Hereditary?
Research suggests that genes play a part in how likely you are to get IBS.
Imagine each gene as a single brick.
One brick alone might not build a wall, but many working together can create a big barrier. That's how genes in IBS work.
Lots of tiny genetic influences, called polygenes, can raise your risk.
In rare cases, a single faulty gene might be the culprit. But for most people, it's a combination of many smaller genetic effects.
Scientists are still figuring out which specific genes are involved, and so far, they've found very few that definitively contribute to IBS risk.
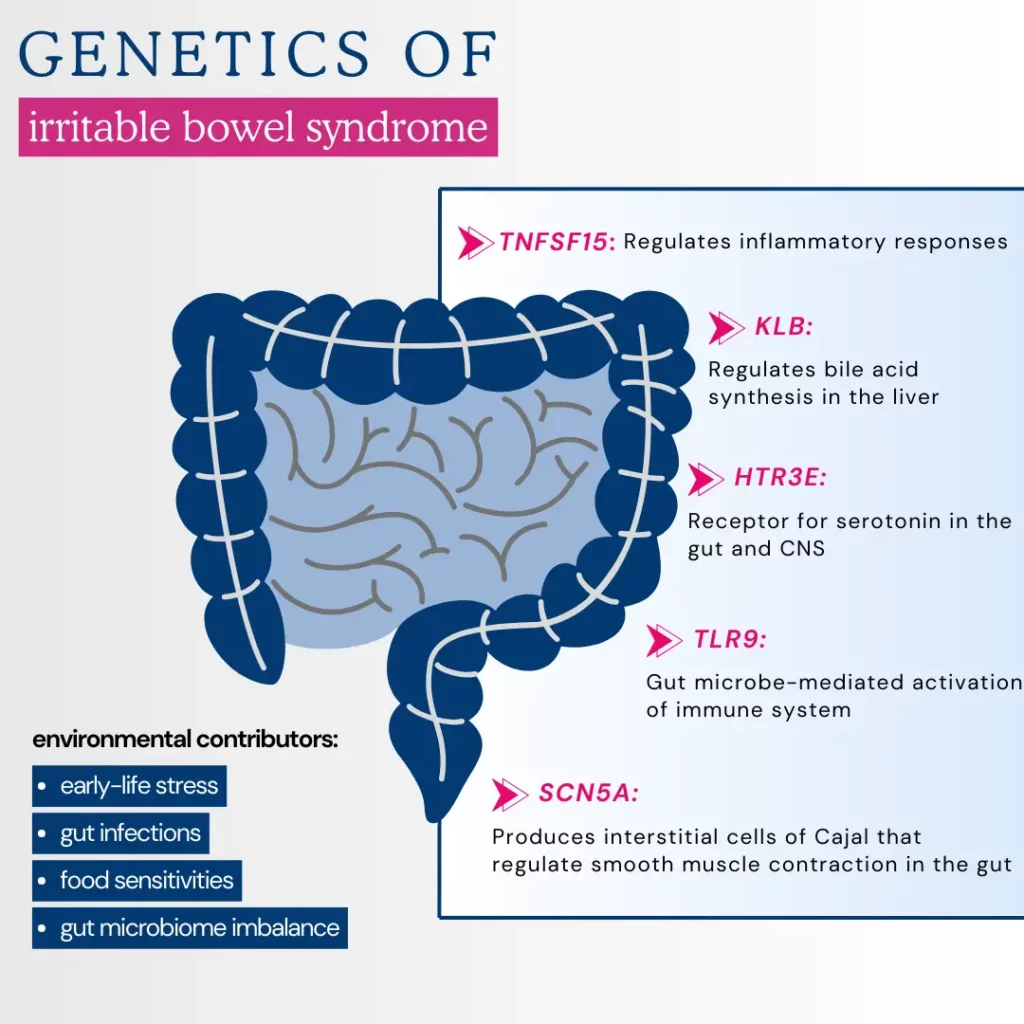
One exception is a gene called TNFSF15, which appears to promote inflammation in the gut.
There's another layer to the story: epigenetics. These are changes that switch genes on or off without altering the actual DNA code.
For example, early life stress might cause epigenetic changes that make you more prone to IBS later on.
While genes influence IBS risk, your environment and lifestyle also play a significant part.
Genes Influencing IBS Risk
Researchers recently conducted a genome-wide association study to identify genes that might influence IBS risk.
This investigation involved over 53,400 individuals with IBS and compared them to a control group of 433,201 participants.
The study identified six specific genetic variations (NCAM1, CADM2, PHF2/FAM120A, DOCK9, CKAP2/TPTE2P3, and BAG6) associated with an increased risk of IBS.
Interestingly, these genes were not directly related to gut function itself. Instead, these genes primarily involve brain function and nerve signaling to the gut.
This finding highlights the importance of the brain-gut axis in IBS.
The study also found a strong correlation between IBS risk and genes associated with anxiety, neuroticism, and depression.
This suggests that shared pathways might underlie both IBS and these mental health conditions rather than anxiety simply causing IBS symptoms.
Further research is needed to understand the exact mechanisms by which these genes influence brain-gut communication in IBS.
Does IBS Run In Families?
IBS appears to run in families, suggesting genetic and environmental influences.
Several studies have explored the familial patterns of IBS, indicating a higher risk among relatives of affected individuals.
Older research from 2008 found a stronger IBS relationship in parents and siblings, especially between mothers and sisters, than in offspring.
This suggests that immediate family members, particularly those with close genetic ties, are at a higher risk.
A 2010 study quantified the strength of family influence, indicating that individuals with relatives who have IBS are 2–3 times more likely to develop the condition themselves.
This study did not find that spouses of those with IBS have a higher risk.
Researchers recognized the clear family association but were uncertain how much was due to genetic factors versus shared household environmental exposure.
Furthermore, a 2014 study found that the risk of IBS is higher among:
- First-degree relatives: Parents, children, and full siblings.
- Second-degree relatives: This category includes uncles, aunts, grandparents, grandchildren, nephews, nieces, and half-siblings.
- Third-degree relatives: First cousins, great-uncles and great-aunts, great-grandparents, and great-grandchildren are considered third-degree relatives.
This suggests a potential genetic influence. However, the study also found that spouses of people with IBS are more likely to have the condition, implying significant nongenetic factors like shared environment or lifestyle.
At What Age Does IBS Appear?
IBS strikes most often in teens and young adults, although it can occur at any age. It's less likely to begin after 50.
Affecting women twice as frequently as men, IBS impacts a significant portion of the U.S. population, with estimates suggesting 10-15% experience its symptoms.
This prevalence makes it the leading reason for gastroenterologist consultations.
Other Contributing Factors To IBS
While genetics play a role in IBS, other factors can significantly influence its development. Since IBS is a functional GI disorder, the focus lies on the gut-brain connection.
Here's what can contribute to IBS symptoms:
- Gut infections: Past infections can leave the digestive system vulnerable, triggering IBS flares.
- Food sensitivities: Certain foods may irritate your gut, leading to IBS symptoms.
- Mental well-being: Anxiety and depression often go hand-in-hand with IBS, suggesting a possible link.
- Gut microbiome imbalance: Shifts in gut bacteria types or numbers can contribute to IBS.
- Early life stress: Traumatic experiences in childhood may increase the risk of developing IBS.
These factors highlight the complex connection between the gut and brain, which causes IBS symptoms.
Is There A Treatment For Hereditary IBS?
Irritable bowel syndrome may lack a permanent cure, but effective management strategies exist to reduce symptoms and improve your quality of life significantly. The specific approach often depends on the severity of your IBS.
Focusing on stress management and lifestyle adjustments can be highly beneficial for milder cases. This might include:
- Identifying and avoiding trigger foods
- Increasing your intake of high-fiber foods
- Staying well-hydrated
- Regular exercise
- Prioritizing sleep hygiene
Dietary changes often involve eliminating:
- High-gas foods
- Gluten
- FODMAPs (specific carbohydrates that can cause digestive issues)
A dietitian can assist in developing a personalized plan to ensure you receive the necessary nutrients.
For more severe IBS, counseling can be a valuable tool, particularly if stress or mental health concerns are contributing factors. Additionally, various medications might be prescribed by your doctor, including:
- Fiber supplements to address constipation
- Laxatives for stubborn constipation
- Anti-diarrheal medications to control diarrhea
- Anticholinergics to relieve cramps
- Antidepressants (tricyclics or SSRIs) to manage pain and regulate gut activity
- Pain relievers for severe pain or bloating
There are also medications specifically designed for IBS, such as:
- Alosetron (for severe diarrhea-dominant IBS in women)
- Eluxadoline (reduces diarrhea by regulating muscle contractions)
- Rifaximin (an antibiotic to target bacterial overgrowth)
- Lubiprostone (increases fluid secretion for constipation, primarily in women with constipation-predominant IBS)
- Linaclotide (enhances fluid secretion to alleviate constipation)
Researchers are exploring fecal microbiota transplantation (FMT), which involves transplanting processed stool from a healthy donor to restore gut bacterial balance.
While still under investigation, FMT holds potential as a future option.
Even with hereditary influences, IBS can be effectively managed through a combination of diet, lifestyle, stress reduction, and potentially medication.
Make sure to always consult a healthcare professional before beginning any treatment plan.
Hand-picked Article For You: 10 Important Signs That Could Indicate An Unhealthy Gut
Can You Prevent Hereditary IBS?
While hereditary IBS cannot be entirely prevented, certain dietary choices may help reduce the risk or alleviate symptoms.
A study released in 2019 via NCBI indicates that polyphenols, with their antioxidant and anti-inflammatory properties, may help protect against IBS.
Polyphenols, found in various foods, have been shown to help protect against gastrointestinal disorders.
Incorporating these polyphenol-rich foods into your diet may lower the risk of developing IBS or lessen its symptoms.
Sources of polyphenols include:
- Fruits
- Vegetables
- Whole grains
- Nuts
- Olive oil
- Tea
- Coffee
Although genetic factors contribute to IBS, adopting a diet rich in polyphenols could be a beneficial strategy in managing and possibly preventing hereditary IBS.
Does Genetic Testing Help With Hereditary IBS Diagnosis?
Despite a possible genetic link to IBS, diagnosing it doesn't involve genetic testing. Instead, physicians concentrate on your symptoms.
They will inquire about persistent stomach discomfort, bloating, and alteration in bowel habits (diarrhea or constipation) that have lasted at least six months.
A physical examination might assist in ruling out other causes, and you may be asked about your family's health history.
Blood and stool tests are also common to exclude other conditions with similar symptoms.
Ultimately, the diagnosis relies on understanding how your pain relates to bowel movements, frequency, consistency, lifestyle, and dietary habits.
So, while genes may be a factor, a DNA swab is optional. Your experience and ruling out other conditions take center stage in diagnosing IBS.
Summary: Is IBS Hereditary?
While IBS can run in families, it's a complex case of inheriting the condition. The answer to "Is IBS hereditary?" is more complicated.
Research suggests genetics contribute to IBS susceptibility. Multiple genes, each with a small influence, can combine to increase your risk.
Interestingly, these genes are more related to brain function and nerve signaling in the gut than gut function, highlighting the mind-gut connection in IBS.
Family studies also show a higher risk of IBS among relatives of affected individuals, but spouses of people with IBS aren't necessarily at higher risk. This suggests environmental factors, like shared diet or stress, might also play a part.
Even with a genetic predisposition, there's hope! Effective management strategies, such as dietary changes, stress reduction, and medication, can significantly improve one's quality of life.
References
https://www.medicalnewstoday.com/articles/ibs-vs-colon-cancer
https://medicalnewstoday.com/articles/is-ibs-genetic
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056499
https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
https://www.nature.com/articles/s41588-021-00950-8
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2873036
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2875200
https://pubmed.ncbi.nlm.nih.gov/24694578
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4752571




