Unlock your genetic potential or gift the power of personalized health. Browse our Supersaver Packs now.
Ayurveda is an ancient system of traditional medicine originating from Indian Hindu philosophies. It is one of the world’s oldest and most continuously practiced systems of medicine. The efficacy of Ayurvedic practices lies in their simple and naturopathic techniques that you can easily try at home. Here are 12 simple Ayurvedic practices that can help improve your overall health and well-being.
Ayurveda comes from the Sanskrit words ayur, meaning life, and veda, meaning knowledge.
Thus, Ayurveda translates to "the knowledge of life".
It is based on three philosophies:
Despite being an ancient system, Ayurveda is still very popular worldwide.
In India, it is considered a separate system of medicine.
Some even treat it as a primary form of healthcare.
In the US, Ayurvedic remedies are used alongside modern medicine.
Here are a few possible benefits of Ayurvedic practices:

A good night's sleep is essential for overall health.
Ayurveda promotes going to bed early (by 10 p.m.) for restful sleep.
Avoid using phones, tablets, or computers in bed or before you fall asleep.
Waking up early the following day is easier if you go to bed early.
According to Ayurveda, sleeping past sunrise can make you feel lethargic all day.
That's why waking up at dawn with eight hours of sleep is the right way to start the day.
Ayurveda promotes drinking optimal quantities of water to balance your bodily functions.
Drink at least eight glasses of water evenly across your day.
Start your day with a warm glass of water to cleanse your gut for easy bowel movement.
It's a common practice to start your day by splashing your face with water.
Interestingly, this is one part of an Ayurvedic practice called Shat Kriya, a gauntlet of six cleansing techniques to harmonize your body and soul.
Abhyanga means massaging your body with warm oil.
It can calm the mind and nervous system, tone your muscles, and hydrate the skin.
A 15-20-minute massage with herbal or medicated oil can be very beneficial in the long run.
The correct order is to start with Yoga, then Pranayama (breathing practice), and finish with meditation.
These relaxation techniques help you feel lighter, starting your day without yesterday’s worries.
Ayurveda recommends three meals a day.
A large, hearty lunch should follow a light, nutritious breakfast.
A simple dinner low in carbohydrates will reduce the load on your digestive system as you wind down for the night.
For a balanced diet, you can follow specific Ayurvedic recipes.
Ayurveda encourages freshly prepared food over canned, packaged, or processed food.
Season your food with herbs, spices, and condiments to aid digestion.
Avoid drinking water or liquids with your food, as it may interfere with digestion.
Your bowel movement can indicate the presence of several underlying chronic conditions and give you an idea about your overall health.
According to Ayurveda, hitting the bathroom first thing in the morning is best for your health.
Cleaner bowels promote long-term gut health.
Good oral health is essential for overall health.
Tongue scrapers, garlic water gargles, herbal toothpaste, and oil pulling are all recommended Ayurvedic techniques for better oral health.
Oil pulling is a mouthwash-like technique that uses an edible oil to cleanse the inside of your mouth.
Simple, homemade concoctions with Ayurvedic herbs can help remedy some common health conditions.
Drinking hot water mixed with ginger and honey can help overcome a common cold.
Applying cinnamon and clove oil to the forehead can help ease migraine symptoms.
These concoctions are safe and easy to prepare on short notice.
Ayurveda promotes well-being and relaxation through consciously performing everyday practices.
A warm bath can be a great way to unwind after a long day.
It relieves stress, helping you prepare for a good night’s sleep.
Ayurvedic diet and lifestyle changes are generally safe, but it’s worth knowing the possible risks of these changes.
The US FDA does not regulate herbal supplements.
Some supplements with Ashwagandha and Triphala may interfere with existing conditions or medications for the same.
Though these supplements are available over the counter, they could be harmful.
Some supplements may contain toxic metals like mercury, lead, and arsenic.
Note: The content of this article is based on currently available information. Consult your healthcare provider before starting, stopping, or continuing any Ayurvedic supplements, treatments, or procedures.
Ayurvedic remedies are simple. You can easily incorporate them into your daily routine. They can improve your overall health and wellbeing in the long run.
While most Ayurvedic supplements are generally safe, some may interact with existing conditions and adversely affect the body. It's always best to consult your doctor before introducing a new diet or supplements.
While Ayurvedic medications can't replace modern medicines, doctors usually prescribe them alongside allopathic, traditional drugs to improve treatment outcomes.

Top 7 Research-backed Ashwagandha Benefits For Men

Is Sleep Meditation For Anxiety Effective?

Top 5 Teas For Better Gut Health In 2024
https://www.everydayhealth.com/integrative-health/ayurveda/guide
https://www.liebertpub.com/doi/abs/10.1089/jmf.2022.0042?journalCode=a
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6492358
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3931197
https://www.healthline.com/nutrition/ayurvedic-herbs
https://www.webmd.com/balance/what-is-pranayama
https://www.hopkinsmedicine.org/health/wellness-and-prevention/ayurveda
https://www.webmd.com/balance/ayurvedic-treatments
Fascinated by what your ancestry tests have revealed? But what if, alongside your results, certain physical traits could add more pieces to your ancestral puzzle? Whether or not Vikings appeared in your DNA report, you might be intrigued to discover which physical signs have historically been associated with these legendary seafarers. Let's delve into 7 fascinating traits that might hint at a Viking connection somewhere in the vast branches of your family tree.
The Vikings were a group of maritime warriors from Scandinavia.
They flourished from the 8th to 11th centuries.
They have left an indelible mark on European history and are known for their expedition to unknown lands.
The Vikings traveled through North America and the Mediterranean in search of fortune.
They established trade connections with European countries like Britain and Ireland.
They also looted monasteries and took whatever money or goods they could.
At the same time, they were accomplished craftsmen who produced jewelry and metalwork that was renowned throughout Europe.
There is some dispute as to where the Vikings were initially from.
However, evidence shows they came from the Scandinavian countries, specifically Norway, Sweden, and Denmark.
One famous instance was when the Vikings attacked the Lindisfarne monastery in Northumbria, England, in 793 CE.
However, Roman scholars referenced warrior groups with features similar to those of the Vikings before this date.
This means that the Vikings were there before 793 CE and probably originated from Scandinavia.
They later emigrated to Britain, Ireland, Greenland, and Iceland.
The Scandinavian peninsula is an area shared by Norway, Sweden, and a part of northern Finland.
Nordic countries refer to all five of the northern European countries.
Researchers sequenced the genomes of 442 human remains recovered from 80 archaeological sites, including Viking burials.
The team focused on collecting samples from teeth and Petrous bones (part of the inner ear), as these preserve DNA particularly well.
Genetic ancestry tests are becoming increasingly popular. While your DNA can be used to learn about your roots, did you know that it can also reveal important things about your health risks and wellness aspects? This allows you to take proactive measures for health conditions, even before the symptoms appear, thereby preventing it. You can upload your DNA data to learn 1,500+ things about your health. Learn more.
Here's how people like you have used their ancestry data to explore Xcode Life
Vikings as a group don't exist anymore.
However, they have Viking descendants all over Europe and the Scandinavian countries.
In many Scandinavian countries, many people dedicate their lives to living like the Vikings did long ago.
There are Viking villages in Norway and Sweden where people recreate the Viking way of life.
In a recent study, scientists examined 300 ancient human genomes from Scandinavia that spanned over 2000 years.
They compared these to modern human genomes and found that nearly 10 percent of Scandinavians had Viking DNA.
In the UK, around 6 percent of people possibly had Viking ancestry.
Many people share their DNA with the Vikings, and a Viking DNA test can help you understand your specific Scandinavian ancestry traits!
These tests examine your DNA and compare it to that of your Viking ancestors to determine how many common segments you share with them; the more segments, the closer you are to the Vikings.
Some companies that offer Viking DNA tests include:
The mutations in the Y chromosome in males indicate the changes that have happened in the direct male lineage.
The two types of mutations are STR and SNP, of which STR is more common.
STRs define the haplogroup as a group of similar haplotypes with a common ancestor.
Among the 20 major Y chromosome haplogroups associated with Vikings are |1, R1a, R1b, G2, and N.
The Vikings hailed from modern-day Scandinavia.
They were also called Norsemen.
People from the Nordic region of Europe are usually considered the closest relatives of Vikings.
The Nordic region consists of Norway, Sweden, and Denmark.
Since the Vikings were seafarers, they traveled to foreign lands across Europe.
As a result, some Viking DNA can also be found among the British, Scottish, and Irish people.
Around 10 percent of people in Sweden and 6 percent in the UK are said to have Viking DNA.
Vikings originally hail from Denmark, Norway, and Sweden.
However, they did travel extensively and conquered the British Isles, including Ireland and Scotland.
It led to cultural exchange and intermingling with the local population.
As a result, Viking DNA can be found in many modern-day Scottish and Irish people.
Having the R1a, R1b, or |1 genetic variation does not confirm that you are a Viking, but you could be related to them.
R1a is commonly found in Eastern Europe, while R1b can be found in Ireland, Wales, France, and Spain.
|1 variation is found in Norway, Sweden, and Denmark.
Outside of these countries, Viking heritage can be found in Britain.
The Vikings colonized and settled in Britain.
If you have any of the above genetic variations with a Norse paternal name, chances are you are related to the Vikings.
Genetic tests usually don't have the word Viking written in the test reports.
The people who take these tests refer to the word "Scandinavia" in the report to claim they are related to the Vikings.
Having Viking DNA can mean that you had a Scandinavian ancestor.
However, people use the results of these genetic tests to explain away specific problematic behaviors.
One man in the US claimed that his Viking ancestry explains why he is so angry all the time.
It is a type of genetic determinism where a person's life results from his genes and is not controlled by him.
The Vikings have long been associated with notions of whiteness and Nordic nationalism.
They have long been used as symbols by prominent fascist movements in Europe.
These genetic ancestry tests can fuel a potential new wave of racism and ethnic chauvinism.
The Vikings are hypothesized to have originated from Scandinavia, which represents present-day Denmark, Norway, and Sweden.
Genetic testing can identify Scandinavian ancestry, which may suggest a link to Vikings, as they originated from this region. However, DNA alone can’t provide definitive proof of Viking descent due to genetic overlap with other European populations.
Many historical accounts suggest that they were generally tall and robust, with fair skin, light or red hair, and blue or light-colored eyes being common.
Historical sources describe some typical traits as prominent cheekbones, strong jawlines, and deep-set eyes.
The blood type of Vikings is not definitively documented, as blood typing was not available at the time. However, studies of Scandinavian populations suggest that they had a mix of blood types, similar to modern populations in the region, with types O and A being the most common.
Historical sources and genetic studies indicate that blue eyes were common among Vikings, especially in northern Scandinavia. However, green and hazel eyes were also present.
Vikings did not have fixed surnames as we do today. Instead, they used patronymic names, meaning they were derived from the father's first name, followed by "son" or "dóttir" (e.g., Eriksson for "son of Erik" or Leifsdóttir for "daughter of Leif").
The Vikings were a group of maritime explorers from Scandinavia.
They conquered and settled in many European regions, leading to cultural intermingling.
Today, their influences can be seen in European art and culture.
Although the original Vikings have long become extinct, their genes can still be found today.
People from Norway, Sweden, and Denmark are said to be most closely related to the Vikings.
Some physical signs like fair skin and tall stature can be linked to having a possible Viking ancestor.
However, claiming a Viking ancestor does not mean anything scientific.
In reality, it can lead to more racial discrimination and ethnic chauvinism.
https://www.theguardian.com/science/blog/2013/feb/25/viking-ancestors-astrology
https://www.cell.com/cell/fulltext/S0092-8674(22)01468-4
https://www.sciencedaily.com/releases/2020/09/200916113544.htm
Founded by Debbie Moon in 2015, Genetic Lifehacks aims to combine an engineering mindset with biological systems and apply genetics to dietary and lifestyle choices. Genetic Lifehacks claims to use people's DNA to optimize their diets and lifestyles based on their needs. This article reviews their website, reports, user experience, and privacy to give a clear verdict. Is Genetic Lifehacks worth it?
Top 5 Topics is a genetic consultation report that analyzes your raw DNA data and studies five main traits of interest.
You can upload your raw DNA in three ways:
The report is usually 12-16 pages long and can cover more than five traits if needed.
It’s worth noting that these five traits are often selected at Debbie Moon’s discretion.
Upon request, the report may focus on specific traits of interest.
You may mention them while completing the order or via email.
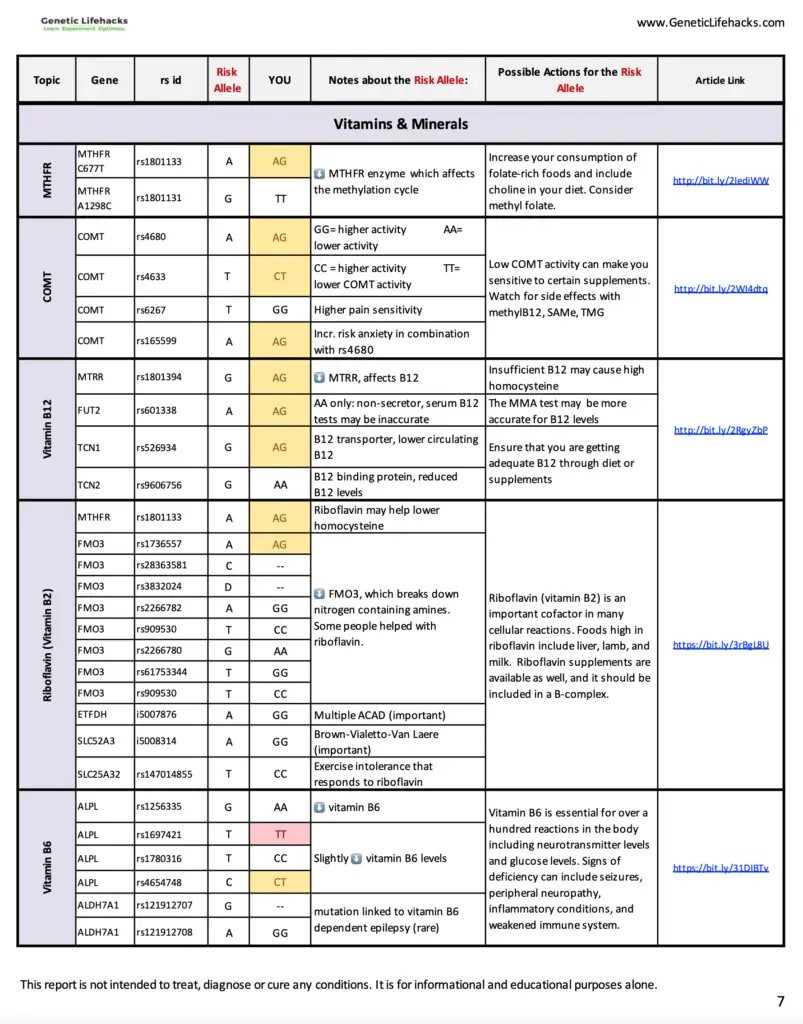
The Genetic Lifehacks Cheat Sheet is a 102-page report of all genetic variants detected in your raw DNA data.
Some of the categories of traits in the Cheat Sheet include:
Its results are presented in a tabular format, mentioning your risk for a given trait and some recommendations for managing it.
Genetic Lifehacks offers a free 4-day email course on the basics of genetics and genetic testing.
The course helps you understand the various facets of a genetic testing report before you purchase one.
You may opt into the course by providing only your email address.
Genetic Lifehacks provides their reports within 2-4 business days.
While their Top 5 Topics report is reasonably concise, at 12-16 pages, their Ultimate Cheat Sheet Report may go up to 102 pages.
This can be difficult to read, especially since their report could be presented in a more readable or user-friendly manner.
Contrary to most other genetic testing services, Genetic Lifehacks displays its results in a tabular column with little room to explain the nature of each trait and the interpretation of each result.
Additionally, please bear in mind that Debbie Moon is not a doctor.
She only provides information and opinions curated using peer-reviewed research and statistics.
It's best to consult a doctor for medical advice regarding the information provided.
Once you subscribe to a membership plan and purchase a product, you can upload your raw DNA data file from 23andMe or AncestryDNA.
The upload process takes about a minute.
Once that is done, you can complete the checkout.
After checkout, you will receive an email with your Top 5 Report within 2-4 business days.
It’s important to note that Genetic Lifehacks doesn’t provide DNA sample kits.
They only accept raw DNA files from 23andme and AncestryDNA at present.
Genetic Lifehacks offers a membership option to its users at the following rates:
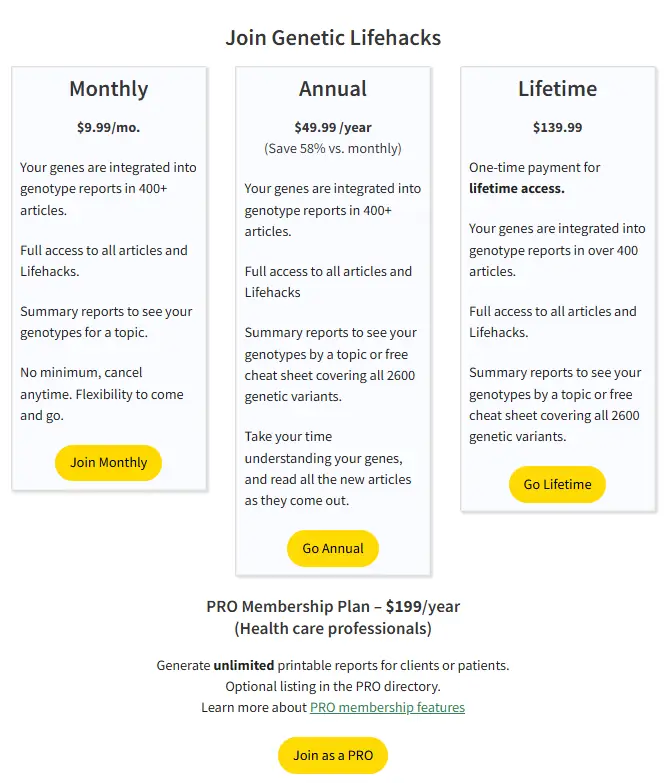
These prices are as of 28th October, 2024. For updated membership pricing, please visit this link.
Genetic Lifehacks offers various services for its users with varied pricing for members and non-members.
For non-members:
For members:
According to their website, Genetic Lifehacks does not store personal information except when purchasing a product.
Additionally, if a user chooses to reach out via email, Genetic Lifehacks records their email address and associated name.
Finally, they store the email addresses of users who opt into their newsletter service.
The website collects user activity statistics and cookies to improve user experience.
To ensure user privacy, they do not use any tracking software on the website.
Genetic Lifehacks has turned off commenting to prevent users from unwittingly sharing sensitive personal and genetic data in the comments under their articles.
Genetic Lifehacks stores user genetic data offline on an encrypted drive.
They delete this data after 30 days and do not use it for research.
The information is used only for consultation and not shared with third parties.
Their privacy policy is transparent about the nature of the information they store and how they handle it.
For further information, read the Genetic Lifehacks Privacy Policy.
More testimonials are available in the News and Research section of their website.
Pros:
Cons:
Genetic Lifehacks has a user-friendly website with a solid community across several forums.
Their email course on genetic testing helps several first-time users understand and appreciate their reports better.
However, the steep cost for non-members, the lack of coverage in reports, and the lack of medical input in each report can deter potential customers.
Genetic Lifehacks may be the right choice if you’d like to learn about a few specific traits and genes in detail instead of receiving an extensive report of dozens of traits.
Genetic Lifehacks may not be the right choice for you if you haven't taken a DNA test yet.
They do not offer a DNA test kit and only accept files from 23andMe and AncestryDNA.
Xcode Life stands apart from other genetic testing companies by providing an efficient, user-friendly, trustworthy, and secure service.
Here's a detailed side-by-side comparison of Genetic Lifehacks and Xcode Life
| Genetic Lifehacks | Xcode Life | |
| Type of genetic testing | DNA raw data analysis | DNA raw data analysis |
| Ancestry reports | Not offered | Not offered |
| Health reports | Not offered | Offered |
| Pharmacogenomic reports | Not offered | Offered |
| Raw data upload | Only from 23andMe and AncestryDNA | DNA raw data from all major providers accepted. Comprehensive list |
| Number of reports | 1 report with 5 topics | 11 |
| Price | Annual membership- $49.99 Other services - $50-$130 No bundles | Reports: $30-$50 Bundles: $160-$199 Price details |
| Sample reports | Nil | Available as detailed report walkthrough videos |
Why are some people more flexible than others? Is flexibility genetic or dependent on your lifestyle? Flexibility is the ability to move your joints and muscles freely through the range of motion that your body allows. In general, body parts that you move more often, like your arms and legs, are more flexible than other parts that aren’t used as much. While exercise can help flexibility, genetics can determine how flexible your joints and muscles can be.
Over-flexibility causes your muscles, ligaments, and tendons to stretch abnormally.
It puts stress on your tendons and ligaments and results in injuries.
Ligaments shouldn’t be stretched beyond more than 6% of their length.
Genetically over-flexible people are at a higher risk of injuries and ligament tears.
While most people think joint mobility depends on your age and how much you exercise, your genes can significantly impact your flexibility.
Some genetic conditions like Ehlers-Danlos may affect your flexibility right from birth.
Certain genes, such as ACTN3, COL5A1, and ESR1, affect the structure and function of muscles, tendons, and ligaments.
Mutations in these genes can take a toll on your flexibility.
How Much Of Flexibility Is Determined By Your Genes?
The levels of flexibility and joint hypermobility vary from person to person, but they are highly hereditable traits with clear genetic links.
Scientists estimate that flexibility is around 50% heritable, meaning that 50% of your flexibility could be thanks to your genes.
The ACTN3 gene helps produce the alpha-actinin protein, which gives structure to muscles in the body.
A 2014 study analyzed the effects of polymorphisms in the ACTN3 gene on flexibility and injury risk in ballet dancers in Korea.
It identified an SNP, rs1815739, that can reduce flexibility if mutated.
Typically, the SNP contains two copies of the C allele.
In some cases, the scientists observed that the C allele was replaced by the T allele, either once or twice.
If both copies of the C allele were replaced by T, flexibility was reduced noticeably.
| Genotype | Outcome |
| CC | Unaffected flexibility |
| CT | Unaffected flexibility |
| TT | Lowered flexibility |
The COL5A1 gene is called the ‘flexibility gene.’
It helps produce type V collagen, which keeps bones, muscles, skin, and tendons strong, mobile, and flexible.
Lowered levels of collagen can result in stiffness and reduced flexibility.
rs12722 is an SNP of the COL5A1 gene.
Similarly to the previous SNP, it usually has the C allele that may be replaced by the T allele.
If the SNP is mutated twice, it will contain two T alleles.
This mutation leads to quadricep stiffness and an increased risk of muscle injuries.
The ESR1 gene codes for an estrogen receptor.
Estrogen influences the production and flexibility of collagen, the tissue found in your ligaments and tendons.
More flexible ligaments equal joints with a better range of motion.
rs2234693 is an SNP of the ESR1 gene.
Like the previous SNPs, the T allele may replace its normal C allele.
Interestingly, with each T allele, muscle flexibility decreases further.
Conversely, each C allele is increasingly protective over muscle flexibility.
Thus, people with the CC genotype are more flexible than those with the CT or TC genotypes, who are more flexible than those with the TT genotype.
Ehlers-Danlos Syndrome (EDS) is a genetic disorder that results in loose joints, very stretchy skin, and overly flexible joints.
People with the syndrome have an extra range of joint movements, also called hypermobility.
EDS can cause joint pain, frequent injuries, and bruises on the skin.
Over 100 mutations in the COL5A1 gene occur in people with EDS.
Since little information exists about the inheritance of flexibility as a trait, scientists have attempted to study the inheritance of the genes that play a role in it.
The ACTN3 and ESR1 genes have complex inheritance patterns; they inherit differently in different cases.
However, the mutations in COL5A1 that lead to Ehlers-Danlos Syndrome are inherited in an autosomal dominant manner.
This means that only one copy of the gene from either parent is sufficient to pass down the condition.
The temperature and time of day- Surprisingly, warmer climates improve flexibility, and you’re generally more flexible in the afternoon than in the morning.
Age- The body's flexibility reduces with age. After 55, collagen production decreases, and tissues lose water, lowering flexibility levels.
Body Bulk - If your body type is bulky, stretching or moving limbs and muscles may be difficult.
Sex: Females are considered more flexible than males because they produce more elastin and estrogen, which are linked to joint flexibility.
Yoga, stretching exercises, pilates, etc., are different exercises that help improve your flexibility.
All these exercises gently stretch muscles and improve mobility.
Static flexible exercises require you to hold a stretch or a position for 30 -60 seconds before relaxing.
They help improve flexibility in different areas of your body.
A warm water bath and breathing exercises can instantly relax your muscles and improve your flexibility.
When done right, massages can help improve flexibility and range of motion.
They can keep your joints more robust and agile in the long term.
Water is essential for the normal functioning of the body.
Dehydration can cause inflexibility and limit your range of motion. Drink enough water every day to stay flexible.
Stress is known to tighten muscles and decrease physical flexibility. Working on mental stress levels can help the muscles relax and improve flexibility.
A naturally inflexible person can become flexible by following a dedicated exercise and stretching regimen. Yoga, pilates, and stretches can slowly build one's range of joint movement.
Flexibility generally increases with age and peaks at age 25. By age 55, collagen production slows down, noticeably decreasing flexibility.
No, stretching cannot increase the length of your bones. It only increases the flexibility and range of movement of your muscles and joints. Height is a complex trait mainly influenced by your genetics and nutrition.
While some genetic mutations can influence flexibility right from birth, non-genetic factors like body type and exercise regimen can significantly impact your overall flexibility and joint hypermobility.

Are Stretch Marks Genetic?

Are UTIs Genetic?

Is Curly Hair Genetic? How DNA Affects Your Hair Type
https://www.frontiersin.org/articles/10.3389/fphys.2017.01080/full
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4241924/
https://medlineplus.gov/genetics/gene/col5a1/#conditions
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4523805/
https://physoc.onlinelibrary.wiley.com/doi/10.1113/EP085974
https://sites.psu.edu/kinescfw/health-education/exercise-articles/the-importance-of-flexibility-and-mobility/
https://www.sciencedirect.com/science/article/pii/S0002929707635290
In 2025, the market is flooded with an array of milk options — from almonds to oats to traditional cow’s milk. But which milk has the most protein content? Dive into this comprehensive review to learn the nutritional profiles of the most popularly consumed types of milk and why you might want to consider switching up your morning pour.
In the world of milk, it is essential to differentiate between dairy and dairy-free options.
While dairy milk predominantly includes that obtained from cows, buffaloes, goats, and sheep, non-dairy milk is predominantly plant-based.
Standard dairy-free milk options are:
There are several reasons why one may want to switch from a dairy to a dairy-free milk option- from allergies and intolerances to sustainability.
Though dairy-free milk options have varying amounts of calcium, vitamin D, and other nutrients, they are often fortified with minerals and vitamins.
Cow’s milk has the most protein compared to many plant-based milks.
According to a new study, while 72% of plant-based milk matches cow’s milk in terms of calcium and vitamin D content, only a few came even close to dairy’s protein levels.
While a cup of cow milk can give you approximately 8-9 g of protein, soy milk comes close, with 7 g of protein for every cup.
Unsweetened almond, soy, and hemp milk have the least amount of carbs.
While whole milk contains all the nutrients, skimmed milk is one with the fat removed.
Processing whole milk to skim milk also causes it to lose some of its other essential nutrients.
Of all the popular dairy and dairy-free milk options today, rice milk is low in fat (one cup contains 2.37 g of fat).
Soy milk is considered to have the highest protein content among dairy-free milk options.
One cup of pea milk contains 6-7 g of protein.
In terms of nutrients, soy milk is the best dairy-free milk option.
This is due to its moderately high protein, calcium, and vitamin D content and low carbohydrate content- all of which are close to that found in cow milk.
Cow's milk giving you tummy troubles? This could be a sign of lactose intolerance! Your ancestry test DNA data includes 700,000 markers, which can be used to learn everything about your nutritional profile, from the most optimal diet for your body to food intolerances. In just 3 steps, you can learn a word of information about your health. Learn more.
| Milk | Calories | Carbs | Protein | Fats | Calcium | Vitamin D |
| Cow’s milk | 259 | 12 g | 9 g | 10.99 g | 300 mg | 0 IU |
| Almond milk | 29 | 3 g | 1.01 g | 2.50 g | 0 mg* | 101 IU |
| Soy milk | 101 | 3 g | 6 g | 3.5 g | 300 mg | 120 IU |
| Oat milk | 130 | 12 g | 4.01 g | 2.5 g | 10 mg* | 101 IU |
| Coconut milk | 76 | 7 g | 0.5 g | 5 g | 130 mg | 42 IU |
| Rice milk | 115 | 22.4 g | 0.683 g | 2.37 g | 288 mg | 8.12 IU |
| Hemp milk | 60 | 3 g | 3 g | 4.51 g | 283 mg | 0 IU |
*While many plant-based milks naturally have low calcium content, most of the manufacturers fortify them with key nutrients like calcium and vitamin D.
For people open to dairy options, cow milk is usually the most recommended by nutritionists worldwide.
If you are a vegan or wish to opt for dairy-free milk, soy milk is the next best option for you.
From a nutritionist’s perspective, cow milk, with the maximum protein and other nutrients, is the healthiest.
The nutrients in cow milk support the growth and development of healthy bones and the body.
If you are planning to go dairy-free, soy milk is comparable to cow milk in terms of protein and nutrition.
Other dairy-free milk options may not be naturally nutrient-rich, but you will find plenty of fortified options.
If you are lactose intolerant and cannot consume cow or other dairy, soy milk is the best for you.
If you are on a weight loss journey and are looking for the best milk option to add to your diet, unsweetened almond milk is the best for you!
According to a study by NIH, unsweetened almond milk has the lowest calories and is a perfect addition to a low-carb diet.
Almond milk is also rich in monounsaturated fatty acids (MUFA) that help achieve weight loss and management.
While dairy options, especially cow milk, have been a staple worldwide for centuries, newer plant-based options are becoming increasingly popular.
In terms of nutrition, dairy-based milk, like those from cows and sheep, contains the highest amount of proteins.
Among dairy-free milk options, soy milk is the closest in terms of nutrition to cow milk.
Prediabetes is more than just a warning sign—it's a call to action. If you've been told you're on the edge of diabetes, it's easy to feel trapped or overwhelmed. But what if there's a way out? With the right knowledge and tools, you can not only halt the progression but actually reverse prediabetes! This isn't just hopeful thinking; it's backed by science and success stories from countless individuals. In this guide, we're going to share the most effective, evidence-based strategies to turn the tide against prediabetes.
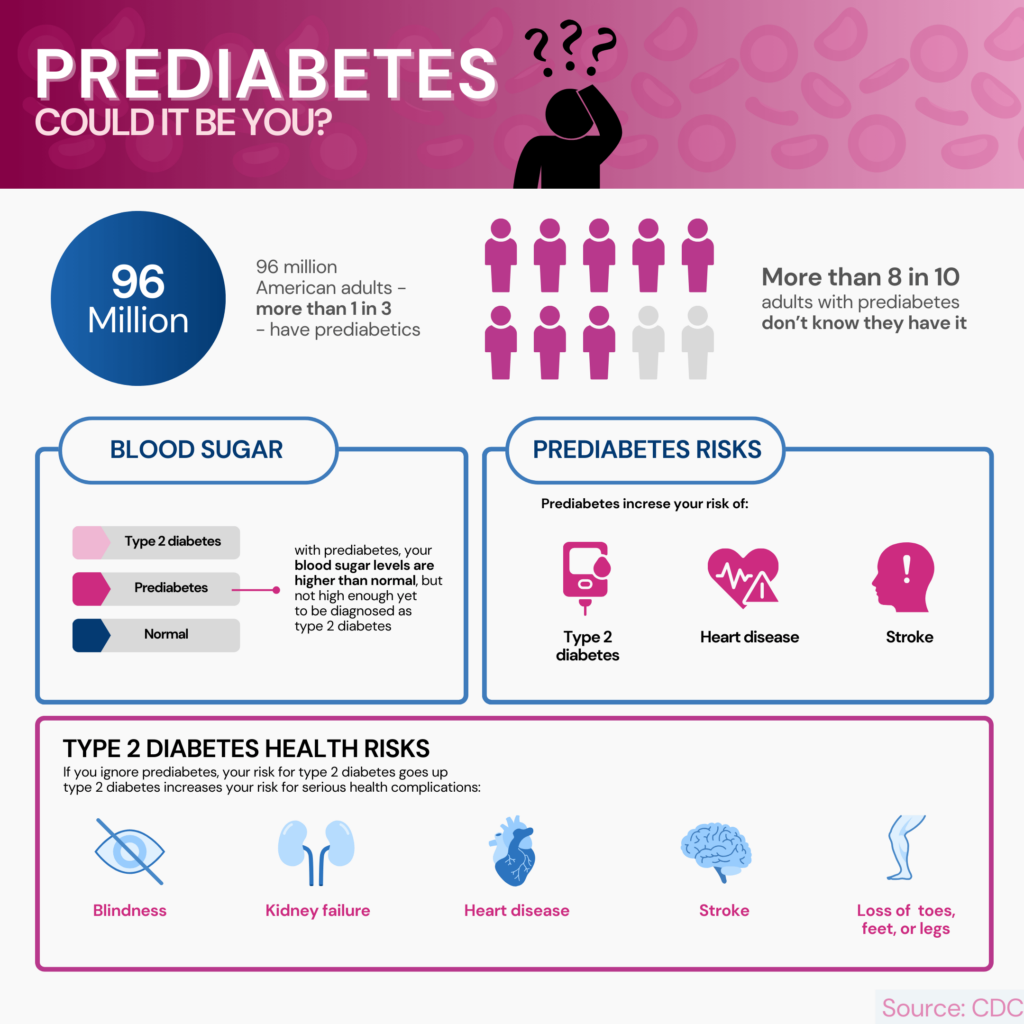
Around 422 million people have diabetes worldwide.
Prediabetes is a precursor to type 2 diabetes.
It is a condition where your blood sugar levels are higher than usual but not as high as someone with diabetes.
It indicates that your body is struggling to check blood sugar levels.
Prediabetes should be taken as it can develop into type 2 diabetes.
1 in 3 adults has prediabetes.
And 8 out of 10 people don’t know that they have the condition.
Having prediabetes and not knowing about it increases the chances of developing type 2 diabetes.
Prediabetes usually shows no symptoms.
Some people, however, can develop a darkening of armpits, elbows, and neck.
A simple blood test result can reveal prediabetes.
Doctors conduct a fasting plasma glucose (FPG) test.
Results anywhere between 100 and 125 can indicate prediabetes.
An A1C test can also detect prediabetes.
This test monitors your blood glucose levels for three months.
Test results between 5.7 and 6.4 can indicate prediabetes.
Prediabetes can develop into diabetes if left untreated.
However, prediabetes is reversible.
Lifestyle modifications can help reverse prediabetes.
Leading a healthy life can significantly reduce the chances of prediabetes developing into type 2 diabetes.
Reversing prediabetes might take several weeks, months, or even a couple of years.
It all depends on the lifestyle changes one makes and how consistent they are with these changes.
Some people might require more time to reverse prediabetes than others.
Those who have diabetes are advised to include and exclude certain foods from their diet to manage the condition.
However, diet is equally important to reverse prediabetes.
Here is a list of foods you should eat and avoid if you want to reverse prediabetes.
Here is a list of foods to include in your diet if you want to reverse prediabetes:
Here is a list of foods that you should avoid if you want to reverse prediabetes:
Exercise is an integral part of every healthy lifestyle.
Lack of physical activity has been linked with diabetes and increased insulin resistance.
Exercising leads to muscles using up stored glucose and maintains insulin sensitivity.
There are different exercises that you can start with.
If you are an absolute beginner, start walking for 30 minutes daily.
Start by doing it twice a week, gradually increasing the frequency.
Once you are ready for more, you can start doing strength training exercises like squats, lunges, or chest presses.
Remember to be consistent with whatever activity you are doing.
Diet and exercise are two of the most important lifestyle changes to reverse prediabetes.
However, there are other things to remember to prevent type 2 diabetes.
Chronic drinking can make your body less sensitive to insulin.
In the long run, this can lead to type 2 diabetes.
People who drink excessive alcohol are advised to drink moderately.
Moderate limits for men are not more than two glasses a day and not more than one for women.
Smoking causes common health problems like heart ailments, cancer, and neuropathy.
Smokers are more prone to develop diabetes from prediabetes.
Around 40% of people who smoke develop type 2 diabetes.
Consult your doctor to control nicotine cravings and quit smoking.
Stress has many adverse consequences for our body.
When you are stressed, your body releases a hormone called cortisol.
Also called the stress hormone, cortisol can increase insulin resistance over time.
It, in turn, will lead to the development of type 2 diabetes.
Stress management techniques are essential to keep your body’s cortisol levels in check.
Stress management is vital to reverse prediabetes.
Sleep plays a vital role in maintaining our overall health.
People who don’t get enough sleep have a higher cortisol level in their blood.
Excess of this hormone can negatively impact the body’s blood sugar levels.
People who don’t get seven to nine hours of sleep will have a higher cortisol level.
People who are chronically awake between 11 p.m. and 5 a.m. can also have higher cortisol levels.
Fixing your sleep schedule can help reverse prediabetes.
Disorders like sleep apnea can also affect the quality of your sleep.
It is a condition where breathing stops repeatedly during the night due to the relaxation of throat muscles.
Consider getting yourself treated if you suffer from this disorder.
Sound sleep will help prevent prediabetes from progressing into diabetes.
Prediabetes usually does not have symptoms.
But if you have any of these risk factors, you might develop prediabetes eventually.
Here are some risk factors you should look out for prediabetes:
Prediabetes has the probability of progressing into type 2 diabetes if left unchecked.
You should consult a doctor if you notice the following symptoms:
There is no sure-shot time frame within which prediabetes can progress into diabetes.
However, certain factors can accelerate the process.
Weight gain or certain medications can make prediabetes progress into diabetes.
Without taking any action, prediabetes can progress into diabetes within five years.
The instances of children developing prediabetes have increased significantly in the last 20 years.
The two main reasons for this development are an unhealthy diet and a sedentary lifestyle.
Eating junk food has led to an increase in total calorie consumption.
Children are suffering from obesity due to unhealthy diets.
Increased screen time has led to less exercise and activity.
These factors are increasingly putting more pressure on the pancreas, the organ that produces insulin and regulates blood sugar.
It has led to more children developing prediabetes.
Changing your lifestyle is probably the only way to reverse prediabetes, but it is gradual.
Once you start to eat a healthy diet and exercise regularly, you will start seeing results.
But test results might take a few weeks to show any improvement.
There is no quick fix to prediabetes, but with consistency, it can be reversed.
Prediabetes is a condition where your body’s glucose levels are higher than usual but not high enough to get a diagnosis of type 2 diabetes.
Prediabetes can progress into diabetes if left untreated.
However, it can also be reversed with lifestyle changes.
A balanced diet and exercise can help reverse prediabetes.
Managing stress and quitting smoking and alcohol are also necessary to reverse prediabetes.
https://www.hopkinsmedicine.org/health/wellness-and-prevention/prediabetes-diet
https://www.cdc.gov/diabetes/library/features/truth-about-prediabetes.html
https://www.healthline.com/health/diabetes/how-to-reverse-prediabetes-naturally
https://www.who.int/health-topics/diabetes#tab=tab_1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914832/
https://www.cdc.gov/diabetes/prevention/about-prediabetes.html