Preeclampsia is a pregnancy complication that affects two hundred thousand pregnant people in the U.S. per year. This worrying number has only been on during and post the COVID pandemic. While certain factors can increase the risk of this condition, research also suggests that family history plays a role here. This article discusses in-depth about preeclampsia, touching upon its risk factors and whether it has any genetic roots.
What Is Preeclampsia?
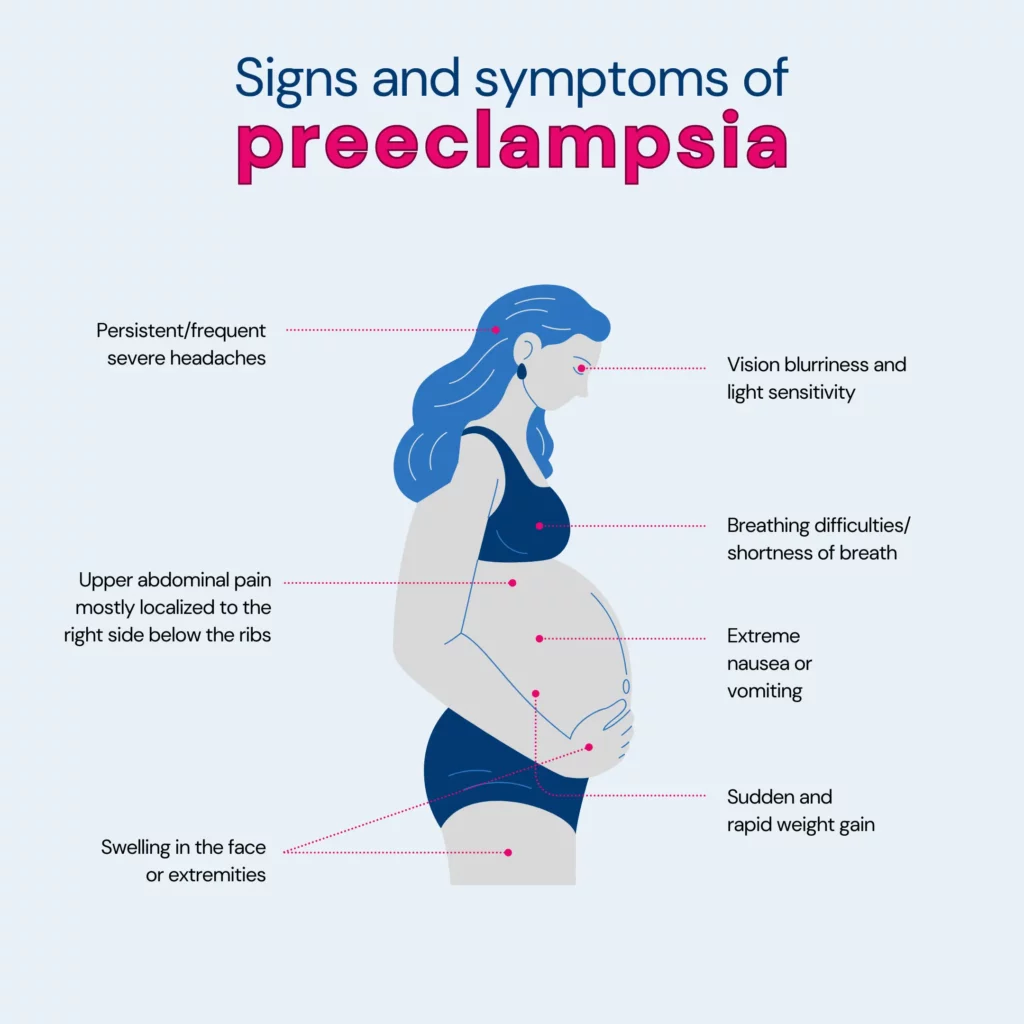
Preeclampsia is a serious condition that may arise during pregnancy, usually occurring after the 20th week.
It results in high blood pressure (hypertension) and is often linked with the presence of protein in the urine (proteinuria), suggesting potential kidney issues.
Preeclampsia can extend its impact to other organs, such as the liver, leading to additional symptoms.
Although it commonly resolves post-childbirth, neglecting treatment can pose significant health risks for both the baby and the mother.
Who Gets Preeclampsia?
Preeclampsia is usually seen in first pregnancies, but if there is a history of it in the previous pregnancy/ies, then the risk of preeclampsia in future pregnancies is seven times higher!
Risk Factors For Preeclampsia
While it can affect anyone who is pregnant, certain factors increase the risk. Let's take a closer look at them:
- Existing health conditions, such as chronic high blood pressure, kidney disease, lupus, autoimmune disorders, or diabetes
- Preeclampsia in a previous pregnancy
- Family history of preeclampsia
Remember, individual risk varies depending on the combination of factors present in each person.
Regular checkups with your healthcare provider throughout the pregnancy are vital steps, ensuring your and your baby's well-being.
Is Preeclampsia Genetic?
Yes, there is substantial evidence suggesting a genetic component in the development of preeclampsia.
Scientists did an extensive study, checking 775 tiny genetic variations in 120 genes of over 350 moms with preeclampsia and 602 without it.
They identified six genes (IGF1, IL4R, IGF2R, GNB3, CSF1, and THBS4) that contribute to preeclampsia development through a combination of maternal and fetal genetic changes.
Can Preeclampsia Run In Families?
Yes, there is a familial link to preeclampsia, indicating a genetic influence on the condition, such as:
- Increased risk with family history:
- Those with a first-degree relative like a mother, sister, or daughter who had preeclampsia are five times more likely to develop it themselves.
- Second-degree relatives affected:
- The risk doubles when there are second-degree relatives (aunt, niece, grandmother) who experienced preeclampsia.
- Insights from twin studies:
- Studies involving twins reveal differences in preeclampsia development, suggesting factors beyond genetics are at play.
- Heritability estimates:
- About 55% of susceptibility to preeclampsia is linked to genetic factors involving maternal and fetal gene contributions.
- Genes under investigation:
- Ongoing research focuses on specific genes associated with fluid balance, vascular function, and placental development in understanding preeclampsia.
Will I Have Preeclampsia If My Mom Had It?
Yes, if your mom had preeclampsia during her pregnancy, there is an increased risk that you may also develop preeclampsia during your pregnancy.
A cohort study involving 22,768 elder daughters and 2,959 younger daughters revealed a link between a mother's preeclampsia and her daughters' vulnerability to it.
Mothers having preeclampsia during the first pregnancy with an elder daughter increase the elder daughter's risk of developing it in her own first pregnancy by 1.7 times. This risk continues into the second pregnancy.
The study found similarly elevated risks for daughters if the mother had preeclampsia in any other pregnancy or if only mothers with firstborn children were considered.
However, it's important to note that genetic predisposition explained only a minor part of preeclampsia occurrence in the population studied.
Is It Possible To Prevent Genetic Preeclampsia?
Preventing genetic preeclampsia isn't guaranteed because it depends on factors beyond your control. However, there are steps you can take to reduce the risk or manage it:
- Prevention:
The best-known method is low-dose aspirin, typically an 81-milligram tablet daily after 12 weeks of pregnancy.
Your primary care provider may recommend this if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
- Lifestyle and healthy choices:
Being as healthy as possible before pregnancy is advised, especially if you've had preeclampsia before.
Manage any conditions that increase the risk of preeclampsia by discussing them with your healthcare provider.
Note: Before taking any medications, vitamins, or supplements, it's crucial to consult your provider to ensure safety.
Health Impacts Of Preeclampsia
Preeclampsia can bring about various health challenges, including:
- Fetal growth restriction: Preeclampsia impacts the blood flow to the placenta, potentially causing slow fetal growth, known as fetal growth restriction.
- Preterm birth: Preeclampsia increases the chances of delivering before 37 weeks, raising risks for the baby, such as breathing issues, feeding difficulties, and developmental delays.
- Placental abruption: The risk of placental abruption, where the placenta separates early, is higher with preeclampsia. Severe cases can lead to dangerous bleeding for both mother and baby.
- HELLP syndrome: An extreme form of preeclampsia, known as HELLP syndrome, can affect multiple organs, posing life-threatening risks to both mother and baby. Symptoms include nausea, pain, and a feeling of illness.
- Eclampsia: Eclampsia involves seizures or coma linked to preeclampsia. Warning signs like severe headaches and vision problems may occur, but sometimes they happen suddenly without any prior symptoms.
- Organ damage: Preeclampsia may harm the kidneys, liver, lungs, heart, or eyes, potentially leading to a stroke or other brain injuries.
- Cardiovascular disease: Having preeclampsia could increase the risk of future heart and cardiovascular issues, especially if it occurs more than once or results in preterm delivery.
Understanding these potential impacts is crucial, and early detection and management are essential for the well-being of both the mother and the baby.
Other Factors That Can Impact Preeclampsia Risk
Additional factors that might slightly raise the likelihood of developing preeclampsia include:
- Women aged 40 or older.
- Women with a history of urinary tract infections.
- Women with obesity (BMI over 35).
- Women carrying twins or triplets.
- Women of African American ethnicity.
- Women with significant spacing between pregnancies (over 10 years).
- Women with single-vessel kidney disease.
- Women with gestational diabetes.
Summary: Is Preeclampsia Genetic?
Preeclampsia is a serious condition during pregnancy with high blood pressure and protein in urine.
It's more likely in first pregnancies, especially if there's a family history or if it happened before.
Genetics is a factor, but it doesn't explain everything. If your mother had it, you're at a higher risk.
Taking low-dose aspirin as prescribed by your doctor and adopting a healthy lifestyle can help lower your risk.
Preeclampsia can cause problems for both mom and baby, so early detection and care are essential.
Age, obesity, and certain conditions can also affect the risk. Regular checkups and healthy choices make a big difference in having a safer pregnancy.
References
https://www.nhs.uk/conditions/pre-eclampsia/
https://www.news-medical.net/health/The-Genetics-of-Pre-Eclampsia.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4060423/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3145161/
https://pubmed.ncbi.nlm.nih.gov/10468424/
https://www.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745




