Varicose veins are a type of vein disorder affecting millions of people worldwide.
According to studies, about 20% of adults will develop varicose veins in their lifetimes.
Varicose veins can cause discomfort, pain and affect the quality of life.
Untreated varicose veins can lead to severe skin and tissue damage.
Various studies report that varicose veins could be hereditary.
These studies have identified multiple gene mutations that may increase the risk of developing the condition.
Did You Know?
Many skin conditions like varicose veins have a genetic component to them. Having certain gene variations can increase your risk for these conditions. Learn more:
What Are Varicose Veins?
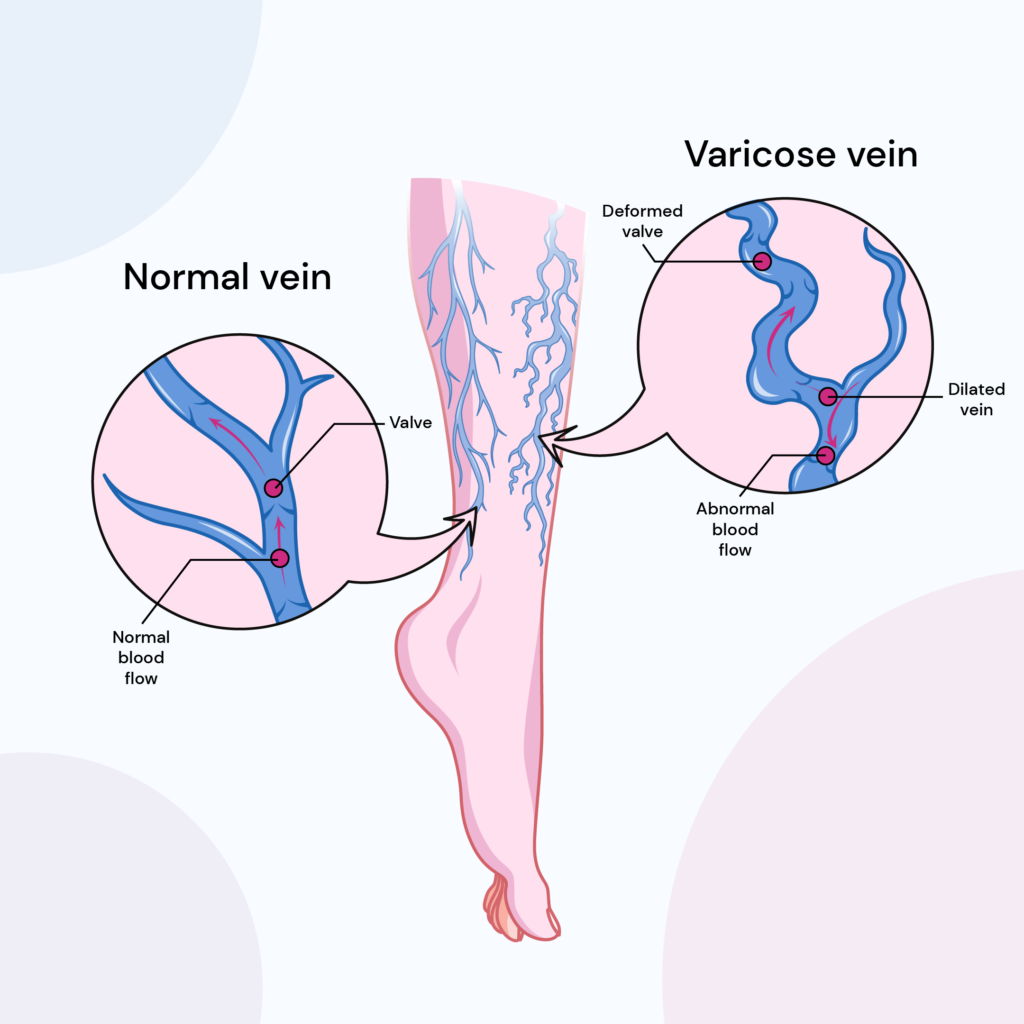
Varicose veins are a condition caused by weak vein valves.
The veins are vessels carrying blood from the rest of the body to the heart for recirculation.
When the vein valves weaken, they cannot carry blood to the heart.
As a result, blood gets collected in the damaged area, and the veins become swollen and twisted.
While this condition can occur anywhere in the body, it is common in the lower extremities.
What Do Varicose Veins Look Like?
Varicose veins are easily identifiable. When the veins swell up or get twisted, the skin around the area turns purple or blue.
The veins may appear twisted or bulged to touch and see.
Other signs of varicose veins include:
- Rashes and sores on the skin
- Burning, itching, or aching feeling
How Are Varicose Veins Caused?
Veins are one-way valves that carry blood from other body parts to the heart.
The walls of these valves can get weak, stretched, and loose for different reasons.
As a result, the veins can’t push blood successfully toward the heart.
As a result, blood pools up, and the veins can enlarge.
When this happens to the veins closer to the skin's surface (superficial veins), the signs are visible.
What Is The Leading Cause Of Varicose Veins?
The most common cause of varicose veins is pregnancy.
During pregnancy, the growing uterus can pressure the blood vessels, slowing blood flow.
Pregnancy-related hormonal changes can also lead to increased blood volume flowing through the veins, leading to vein enlargement.
A 2016 meta-analysis reports that pregnant women are at 82% higher risk of developing varicose veins than non-pregnant women.
Other common causes of varicose veins are excess weight and standing for long periods.
Risk Factors For Varicose Veins
The following are some of the risk factors for developing varicose veins.
Gender - women are at higher risk for developing varicose veins than men. Pregnancy is an added risk factor in women.
Age - as people age, the blood vessels weaken, increasing the risk of developing varicose veins.
Genetics - inherited genes are a critical risk factor for varicose veins. Studies report that between the parents, mothers have a higher chance of passing on varicose veins gene mutations to children than fathers.
Body Weight - excess body weight stresses the circulatory system, and the veins must work harder to push blood toward the heart. This can weaken the vein walls, increasing the risk of developing varicose veins.
Studies report that obesity increases the risk of developing varicose veins and the severity of the condition.
Occupation - some jobs require the person to keep standing for extended periods, which can increase the risk of developing varicose veins.
Height - a 2018 Stanford article reports that height may be a risk factor for developing varicose veins.
Are Varicose Veins Hereditary?
Apart from age and gender, genes remain a significant risk factor for developing varicose veins.
A 2019 community-based clinical study analyzed the genes responsible for causing varicose veins in about 500,000 individuals in the UK.
According to this study, about 30 independent genetic variants could cause varicose veins.
These can be inherited from either of the parents.
Do Varicose Veins Run In Families?
A 2009 study report that in the case of positive family history, men have a 30% chance, and women have a 56% chance of inheriting the condition.
Without a family history, the risk reduces to 7% in men and 22% in women.
Another older study conducted among Japanese women reports that 42% of women with varicose veins have a family history of the condition.
So, varicose veins run in families.
According to a French study, the risk may increase by up to 90% if both parents have the condition.
So, overall, there’s compelling evidence that suggests that varicose veins have a hereditary factor and that the risk can run in families.
The Role Of Genes In Varicose Veins
The following are major genes associated with varicose veins in humans.
CASZ1 gene
The CASZ1 gene (castor zinc finger 1 gene) produces the CASZ1 protein.
Mutations of this gene are associated with blood pressure variations.
rs11121615 is a Single-Nucleotide Polymorphism (SNP) in this gene. The T allele of this SNP increases the risk of developing varicose veins.
THBD gene
The THBD gene (thrombomodulin gene) is responsible for producing the THBD protein.
THBD gene mutations may alter vein function and increase the risk of developing varicose veins.
Other genes associated with varicose veins are PIEZO1, PPP3R1, GATA2, HFE, and EBF1.
Genetic Test To Identify My Risk For Varicose Veins
If you have taken an ancestry genetic test (from companies like 23andMe and AncestryDNA), you can upload your DNA data to receive varicose veins report.
Varicose Veins + 22 Other Traits In Gene Skin Report
How To Prevent Varicose Veins?
- Reduce excess weight
- Stay physically active
- Avoid standing for long periods
- Keep the feet elevated while sitting
- Avoid wearing tight-fitting clothes
Treating Varicose Veins
- Compression Stockings - using compression stockings help put pressure on the veins and prevent vein enlargement and blood pooling. Doctors may recommend using these stockings every day.
- Vein Stripping - vein stripping is surgically removing the affected veins.
- Sclerotherapy - in this process, saline solution is injected into the affected veins, causing narrowing of the veins. As a result, the veins close down, and the healthier veins around take over the job of carrying blood. This is a minimally invasive treatment for the condition.
- Thermal Ablation - laser therapy is used to destroy the affected veins. This allows for other healthier veins to take over.
- Microphlebectomy - small incisions are made on the skin, and the affected veins are cut and removed.
Can Varicose Veins Be Reversed?
In most cases, it is not possible to reverse the vein wall damage.
Treatment involves removing or making the affected veins dormant so the other healthier veins can carry blood in that area.
Summary: Are Varicose Veins Hereditary?
There are more than 30 genes identified that may cause varicose veins.
When either or both parents have varicose veins, the children are more likely to inherit them.
Gene mutations and other risk factors determine whether a person develops varicose veins and the intensity of the condition.
When genetic testing puts a person at a higher risk for developing varicose veins, lifestyle changes like losing weight and staying physically active may help prevent or postpone the development of the condition.
References
- https://www.ncbi.nlm.nih.gov/books/NBK279247/
- https://pubmed.ncbi.nlm.nih.gov/27639009/
- https://pubmed.ncbi.nlm.nih.gov/15156127/
- https://pubmed.ncbi.nlm.nih.gov/18313335/
- https://pubmed.ncbi.nlm.nih.gov/31570750/
- https://www.ahajournals.org/doi/10.1161/circulationaha.106.675348
- https://www.genecards.org/cgi-bin/carddisp.pl?gene=CASZ1
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6400474/
- https://www.sciencedaily.com/releases/2018/09/180924091649.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6490943/
- https://www.ahajournals.org/doi/10.1161/CIRCGENETICS.112.963439