Did you know that approximately 39 million U.S. adults and 936 million people worldwide suffer from a serious form of sleep apnea? With snoring affecting up to 94% of patients, it’s clear that sleep apnea is a widespread issue. But what if your genes influence your risk of developing sleep apnea? Are certain people more likely to suffer from this condition due to inherited traits? And how can you manage and treat sleep apnea if it runs in your family? In this article, we delve into whether sleep apnea is genetic, explore the risk factors, and review the most effective treatments.
Sleep Apnea: An Overview
Sleep apnea is a disorder characterized by frequent interruptions in breathing during sleep, called apneas, which can last from a few seconds to a minute.
These interruptions disrupt sleep patterns, resulting in fragmented and poor-quality sleep.
The condition can lower blood oxygen levels, straining the cardiovascular system.
Sleep apnea is often undiagnosed because it occurs during sleep, and the individual may be unaware of it.
It is a severe condition that requires medical intervention to prevent long-term health complications.
Types Of Sleep Apnea
Sleep apnea is generally classified into three primary categories:
- Obstructive sleep apnea (OSA) occurs more often than other types, affecting a substantial 39 million Americans and 936 million people worldwide. It occurs when the throat muscles relax and block airflow into the lungs.
- Central sleep apnea (CSA) is less common and happens when the brain doesn't send proper signals to the muscles that control breathing.
- Treatment-emergent CSA, also called complex sleep apnea, happens when someone with OSA develops CSA during therapy for OSA.
Symptoms
Sleep apnea presents a variety of symptoms, which can differ in their visibility and impact. Key signs include:
- Frequent nighttime awakenings due to interrupted breathing
- Daytime fatigue and sleepiness
- Snoring
- Mood changes (depression and anxiety)
- Cognitive issues (memory loss, trouble concentrating, etc.)
- Insomnia
- Night sweats and restlessness
- Sexual dysfunction
- Morning headaches
Sleep apnea can exhibit different symptoms in children, including:
- Hyperactivity or focus issues (symptoms similar to ADHD)
- Loud snoring
- Bedwetting
- Unusual movement and positions while asleep
- Reflux or night sweats
Recognizing these symptoms can help diagnose and manage sleep apnea effectively.
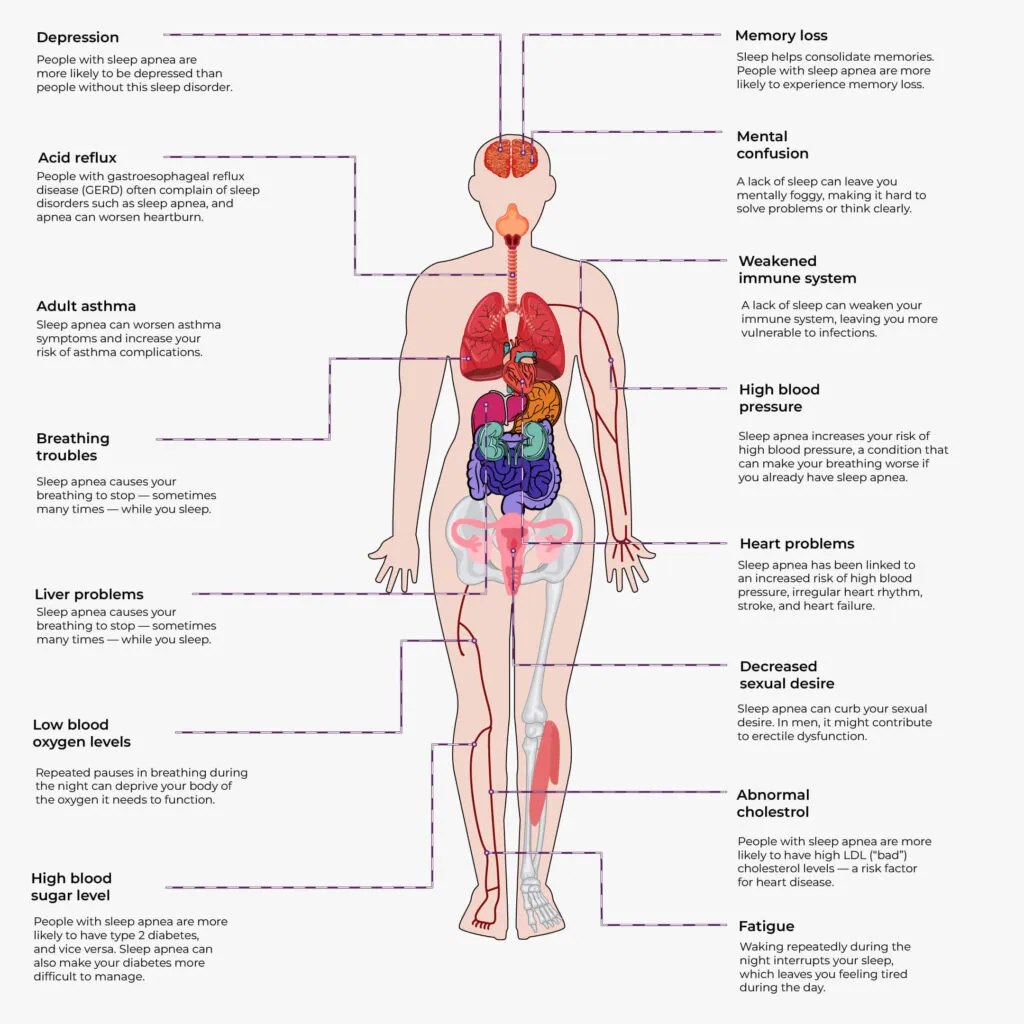
Side Effects Of Sleep Apnea
Is Sleep Apnea Genetic?
Sleep apnea is a complex trait that has genetic, lifestyle, and environmental influences. No single gene causes sleep apnea. However, the effect of small variations (or changes) in multiple genes combined together can increase the risk of sleep apnea.
Central vs. Obstructive Sleep Apnea
| Type of sleep apnea | Genetic link | Details |
| OSA | Strong | Multiple genes contribute to OSA development. Genetics account for approximately 40% of the variation in OSA severity. |
| CSA | Weaker | Possible genetic predisposition, but primarily caused by non-genetic factors like brain respiratory control issues. More research is needed. |
How Is Sleep Apnea Inherited?
Central vs. Obstructive Sleep Apnea
CSA is not known to be inherited, but OSA can run in families. If a parent, sibling, or child has OSA, you’re about 50% more likely to develop it yourself.
CSA is often linked to other medical conditions or certain medications.
In contrast, OSA is linked to genetic traits that affect the structure of your airway, and certain inherited physical features can increase your risk of developing it.
Genetic Factors That Indirectly Contribute To Sleep Apnea
Genetic factors can influence several physiological traits that increase the risk of OSA.
These factors do not directly cause sleep apnea but can make someone more likely to get it.
Key contributors include:
- Narrow throat
- Receded lower jaw
- High-arched hard palate
- Unusually long soft palate
- Large or long tongue
- Excess fat around the neck area
- Large tonsils
- Hypothyroidism
- Obesity
Genes Involved In Sleep Apnea
Several genes have been identified as potentially related to sleep apnea:
- Prostaglandin E2 receptor EP3 subtype (PTGER3)
- Angiopoietin-2 gene (ANGPT2)
- Dopamine receptor D1 encoding gene (DRD1)
- Lysophosphatidic acid receptor 1 (LPAR1)
- β-arrestin 1 gene (ARRB1)
- Tumor necrosis factor-α (TNFα)
- Serotonin receptor encoding gene (HTR2A)
- G-protein receptor gene (GPR83)
These genes are linked to physiological processes influencing OSA risk, including responses to hypoxia and airway muscle tone regulation.
Further research is needed to fully understand the role of these genes and their interactions in the development of sleep apnea.
About Xcode Life's Gene Sleep Report
What Is The Root Cause Of Sleep Apnea?
The root cause of sleep apnea varies depending on its type.
- For OSA, it's when something blocks your airway, like obesity, large tonsils, or changes in hormone levels.
- For CSA, it's when your brain doesn't send the right signals to breathe.
Other Risk Factors For Sleep Apnea
Multiple factors can heighten the risk of developing sleep apnea, including both obstructive and central forms:
- Age: Risk increases with age due to changes in body tissue and respiratory control.
- Heart and kidney conditions: Heart and kidney failure can cause fluid buildup in the neck, potentially obstructing the airway.
- Lifestyle choices:
- Smoking: Causes inflammation in the upper airway, affecting breathing.
- Alcohol: Can relax throat muscles and block the airway.
- Sex at birth: Males are more likely to develop severe sleep apnea at a younger age compared to females.
- Opioid use: Long-term use or disorder related to opioids can disrupt brain control over breathing.
- Health conditions:
- Neurological and muscular conditions such as stroke, ALS, or myasthenia gravis can affect breathing control.
- Hormonal imbalances can also impact respiratory function.
- Premature birth: Infants born before 37 weeks may have a higher risk of sleep-related breathing problems, which generally decreases with age.
Is It Possible To Prevent Genetic Sleep Apnea?
You can't control your genes, but you can control your lifestyle. Even if you're genetically predisposed to sleep apnea, making healthy choices can significantly lower your risk.
Key measures include:
- Avoiding alcohol
- Avoiding sleep medications*
- Avoiding muscle relaxers*
- Quitting smoking
- Losing weight
- Exercising regularly
- Sleeping on your side instead of your back
- Following a heart-healthy diet
- Developing healthy sleeping habits
*The contents of the article are for informational purposes only. Do not stop any medications without consulting your medical practitioner.
Management And Treatment Options For Genetic Sleep Apnea
Genetic sleep apnea, involving inherited factors that affect the upper airway or respiratory control, can be managed through a combination of lifestyle changes.
Even with its genetic basis, various treatment options exist to address this condition effectively.
Here's an overview of treatment options for genetic sleep apnea:
- Continuous positive airway pressure (CPAP) therapy
- Provides a constant stream of positive pressure air through a mask to keep the airway open
- Adjustable mask and settings to enhance comfort
- Adding moisture to the air can alleviate nasal symptoms
- Surgery
- Procedures to widen the airway by stiffening, shrinking, or removing obstructing tissue or enlarged tonsils
- May be performed in a doctor's office or hospital, depending on the procedure's extent
- Mandibular repositioning device (MRD)
- Custom-made oral appliance suitable for mild or moderate OSA
- Keeps the jaw positioned forward during sleep to maintain an open upper airway
- Possible side effects include jaw or tooth pain and may worsen temporomandibular joint disease
- Medication
- Certain medications may help with CSA under the guidance of a sleep specialist
- Examples include acetazolamide, zolpidem, and triazolam
- May cause significant adverse reactions and might not be suitable for everyone
These management and treatment options can help individuals with genetic sleep apnea lead healthier lives by improving breathing during sleep and addressing related health concerns.
Summary
- Sleep apnea disrupts breathing during sleep, lowering blood oxygen and straining the heart.
- There are three types—OSA, CSA, and treatment-emergent CSA.
- OSA occurs when airways are blocked; CSA happens when the brain fails to signal breathing.
- Symptoms include fatigue, snoring, cognitive issues, and frequent awakenings.
- OSA can be genetic, while CSA is linked to other conditions and medications.
- Genetic factors for OSA include a narrow throat, large tonsils, and obesity.
- Essential genes involved include PTGER3, ANGPT2, DRD1, LPAR1, ARRB1, HTR2A, and GPR83.
- Root causes include airway blockages for OSA and brain signal issues for CSA.
- Risk factors consist of age, heart conditions, smoking, alcohol use, and obesity.
- Prevention methods involve lifestyle changes such as quitting smoking, losing weight, and maintaining healthy habits.
- Treatment options involve CPAP therapy, surgery, mandibular devices, and medications.
Others Are Also Reading

Can Sleep Apnea Lead To Brain Damage?

Sleep Issues: Why Do I Keep Waking Up At 4 AM?

The Top 3 Methods To Fall Asleep Faster
References
https://www.ncoa.org/adviser/sleep/sleep-apnea-statistics
https://www.nhlbi.nih.gov/health/sleep-apnea
https://www.mayoclinic.org/diseases-conditions/sleep-apnea/symptoms-causes/syc-20377631
https://my.clevelandclinic.org/health/diseases/8718-sleep-apnea
https://www.medicalnewstoday.com/articles/317313
https://www.webmd.com/add-adhd/attention-deficit-hyperactivity-disorder-adhd