A new study conducted by the researchers at Mount Sinai reports that certain metrics related to inflammation collected from wearable devices metrics can help predict an IBS flare-up. “However, these changes are likely not specific to one disease,” cautions Robert Hirten, MD, the first author of this study.
The 101 Of IBS
Irritable bowel syndrome (IBS) is a group of conditions that affect the gastrointestinal tract - namely, the stomach and intestines.
It is characterized by symptoms like excess bloating and gas, diarrhea, constipation, and abdominal cramps.
Suma Magge, MD, a gastroenterologist at Norwalk Hospital, says that IBS can be subdivided into diarrhea-predominant irritable bowel versus constipation-predominant irritable bowel or even a mixed picture.
- IBS-C: IBS with constipation
- IBS-D: IBS with diarrhea
- IBS-M: IBS with constipation and diarrhea
Scientists still don’t know exactly what causes IBS.
Food intolerances, stress, certain medications, genetic predispositions, and even gut bacteria imbalances are all possible culprits.
There’s also a growing consensus that nerve endings in the gut may be extra sensitive in people with IBS.
How Can A Smartwatch Predict IBS Flareup?
Wearable devices track various physiological metrics that can indicate changes in health status.
Four in particular caught the Mount Sinai team’s attention:
- Heart Rate (HR)
- Heart Rate Variability (HRV)
- Oxygen Saturation (SpO2)
- Activity Levels
Taken together, these measurements can offer a window into your overall inflammation status.
Subtle changes in any of these metrics, even weeks before you feel any discomfort, might suggest that your body is heading toward a flare.
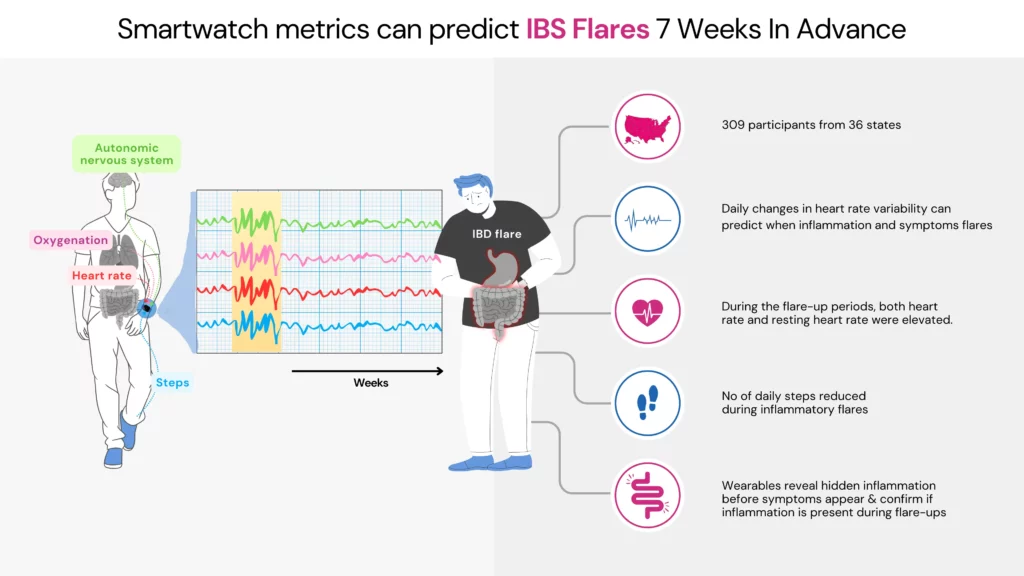
Inside The Study
Mount Sinai researchers conducted this study on 309 participants across 36 states, all of whom had either ulcerative colitis or Crohn’s disease.
The participants were made to wear an Apple Watch, Fitbit, or Oura Ring and answer daily symptom surveys.
They also provided periodical blood and stool samples for assessment.
The wearable devices collected information on HR, HRV, SpO2, and activity levels.
The study was conducted from December 2021 until June 2023.
What They Found
Up to seven weeks before people showed any indication of a flare — whether an inflammatory marker in blood tests or actual GI symptoms — these four wearable measurements had already started drifting from their baseline values.
| Phase | Heart Rate | Resting Heart Rate | Daily Steps |
| Inflammatory flares | Higher | Higher | Lower |
| Normal periods | Normal baseline value | Normal baseline value | Normal activity |
Why This Research Matters
IBS often goes undiagnosed for an estimated 75% of cases.
And even if you do know you have it, there hasn’t been a great way to anticipate a flare.
Typically, you just start feeling abdominal discomfort right before the flare hits, leaving little to no time to intervene.
Early warning signals from wearables could change that.
If you know a flare is likely in a week or two, you (and your care team) might adjust your diet or medication before symptoms actually strike.
Dr. Hirten told Medical News Today that this method could potentially be applied to other chronic inflammatory conditions like rheumatoid arthritis. He also added that their goal is to develop AI-powered algorithms that crunch your wearable data in real-time to warn you — and your doctor — that trouble’s brewing.
We recommend the Genome Pack! Rated 4.7/5 By Users Like You
This report is not a diagnostic tool but a resource to help you better understand your genetic tendencies. Combined with advice from a healthcare professional and other diagnostic methods, it can guide more informed lifestyle and dietary choices. Xcode Life doesn't ship out DNA kits.
Tips To Prevent/Manage IBS Flareups
“Everyone’s IBS triggers are as unique as a fingerprint,” explains Christine Lee, MD, a gastroenterologist at the Cleveland Clinic.
Maybe it’s stress, a missed night of sleep, a new medication, or one of countless possible diet tweaks.
Identifying Triggers
Start a simple journal (or use a symptom-tracking app) to note what you eat, how you feel, and any stressors or schedule changes. Patterns often emerge faster than you think.
Beyond triggers, experts also emphasize a few key lifestyle tips:
Staying Active
Exercise is considered the best medicine for IBS management because regular movement improves circulation, supports digestive function, and helps reduce stress.
Prioritizing Quality Sleep
Dr. Magge says, “If you don’t have enough sleep, the effects of that could accentuate the symptoms of IBS.”
Maintaining a regular bedtime, avoiding late-night screen time, and making your bedroom as comfortable as possible can help calm an irritable bowel.
Staying Hydrated
Staying hydrated throughout the day promotes normal bowel function.
Inadequate water intake can lead to constipation and other digestive issues, so make sure you’re drinking enough fluids.
Monitoring Caffeine Intake
While some people can sip coffee without a problem, others find that caffeine aggravates their symptoms.
Track how you feel after consuming caffeinated beverages. If you notice a pattern of discomfort, consider reducing or eliminating caffeine.
Bonus Tip: Two Expert-recommended Diet Strategies That May Help Your IBS
Dr. Bedford recommends eating plans along the lines of the Mediterranean diet as a good choice for people with IBS.
- Inclusions: Fruits and vegetables, nuts and seeds, whole grains, fish and seafood, greek yogurt
- Exclusions: Red meat, refined grains, processed foods, saturated fats in excessive amounts
Dr. Magge suggests the low FODMAP diet—fermentable, oligosaccharides, disaccharides, monosaccharides and polyols—that can help reduce bloating, gas, and diarrhea.
- Inclusions: Certain fruits like berries, cantaloupes, and citruses, vegetables like carrot, celery, cucumber, eggplant, lettuce, potatoes, zucchini, and pumpkin, lean meats, eggs, poultry, tofu, gluten-free pasta, lactose-free milk
- Exclusions: Fruits like apples, mangoes, peaches, and plums, vegetables like artichoke, asparagus, broccoli, Brussels sprouts, leek, onion, mushrooms, milk, most cereals
Note: For those with IBS, any changes to their diet should be done only under the guidance of a healthcare professional.
The Bottom Line
While your smartwatch can’t diagnose you or cure you, it might soon be able to offer a heads-up before your gut decides to revolt. That could be the difference between catching a flare early — with small, strategic lifestyle or medication tweaks — and dealing with a full-blown, day-ruining attack.
As technology advances, combining wearable data with tried-and-true IBS management strategies may give you a proactive edge. In the meantime, keep listening to your body, stay on top of stress, and team up with your healthcare professionals to get ahead of (and maybe even outsmart) those IBS flare-ups.
References: Original Article
https://www.gastrojournal.org/article/S0016-5085(25)00013-7/abstract




