Disclaimer: This blog post is for information purposes only and must not be taken as medical advice. Please consult a qualified medical practitioner for appropriate treatment.
As if menstrual cramps and bloating weren't enough, for many women, migraines can also strike during their period. But why exactly does this happen? A new study has shed light on the matter, revealing some fascinating insights into the link between hormones and headaches.
What Are Hormonal Headaches?
Hormonal headache is linked to hormonal fluctuations in the body.
They are most commonly associated with changes in estrogen levels, which occurs during the menstrual cycle, pregnancy, and menopause.
Hormonal headaches range from mild to severe and can often be accompanied by other symptoms such as nausea, sensitivity to light or sound, and fatigue.
Women are more likely than men to experience hormonal headaches and often find their headaches more frequent or severe during certain times of the month.
Menstrual Migraine
Menstrual migraine is a specific type of hormonal headache that occur in women in the days leading up to or during their period.
These migraines are often more severe and longer-lasting than a typical migraine.
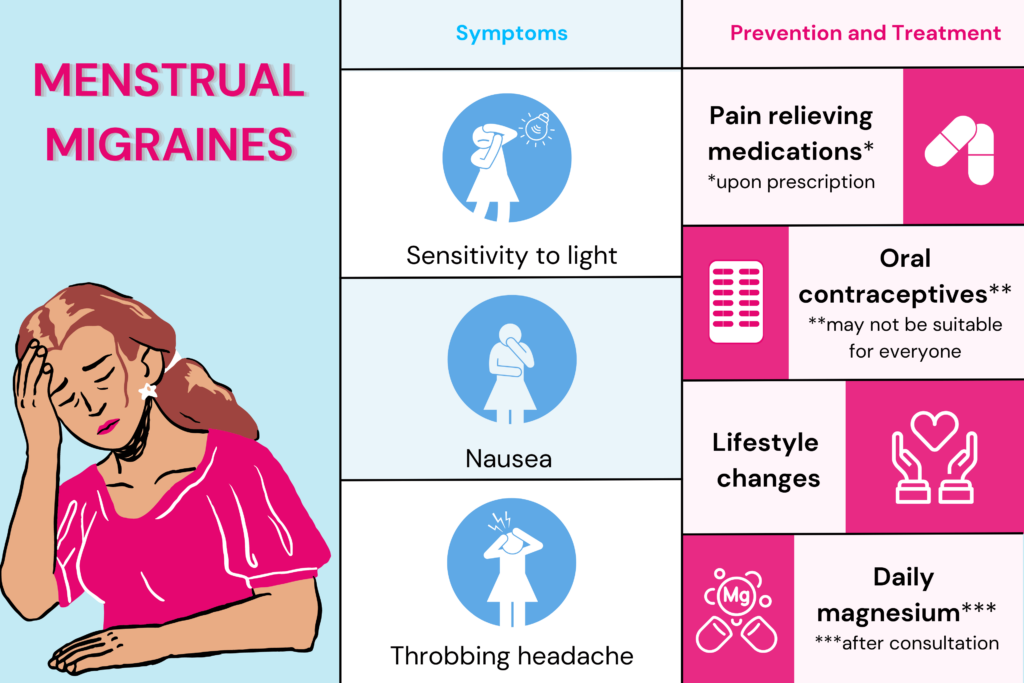
Symptoms include nausea, vomiting, and sensitivity to light and sound.
The exact cause of menstrual migraines is not fully understood, but it is believed to be related to changes in estrogen levels.
As estrogen levels drop before and during menstruation, it can trigger the release of certain chemicals in the brain that can cause migraine.
Women who experience menstrual migraines may benefit from tracking their menstrual cycle.
What Causes Migraine During Your Periods?
A study published on February 22, 2023, in the online issue of Neurology explored the cause behind attacks experienced by cisgender women during periods.
Study Details
Study Participants
Three groups of 30 (total of 90) cis-gendered women with episodic migraine was considered for this study.
They all experienced migraines for at least three days in the month before the study.
The group included those with regular menstrual cycles, those on oral contraceptive pills (OCPs), and those who had gone through menopause.
Three groups of 30 cis-gendered women, each without migraines, were considered for reference.
Study Design
The researchers measured the levels of a protein called CGRP (calcitonin gene-related peptide).
When CGRP is released, it results in the inflammation of the protective layer of the brain called the meninges.
This can result in a migraine attack in some.
To measure CGRP levels, the researchers collected blood and tear fluid samples.
The samples were collected around ovulation time (CGRP levels highest) in those with regular menstrual cycles.
For those on OCPs, sample collection was done during hormone-free and hormone-intake time.
Sample collection was at random times for those who attained menopause.
Study Observations
For those with migraines and regular menstrual cycles, CGRP levels were higher during menstruation than those with migraine - 5.95 pg/ml in the former group and 4.61 pg/ml in the latter group.
For those on OCPs and those who attained menopause, the CGRP levels weres similar between the migraine and non-migraine groups.
Study Conclusion
The increase in CGRP levels following estrogen fluctuations can help explain why migraines are more likely to occur during periods and why the attacks decline post-menopause.
Study Limitations
Accurate blood measurement of CGRP levels is challenging due to its short half-life.
CGRP measures through tear fluid are non-invasive but still exploratory.
The hormone levels were considered around ovulation time; however, they may not have been taken on the exact day of ovulation.
So the full extent of estrogen level fluctuation may not have been captured.
How To Prevent Menstrual Migraines?
There are several strategies that women can use to help prevent and manage period migraines.
Pain Relieving Medications
Triptans are a type of specific painkiller for migraine. They work by calming down overactive pain nerves.
Nonsteroidal anti-inflammatory drugs, or NSAIDs, like naproxen, can also be used to get relief from pain.
NSAIDs are also used as prophylactic drugs - to prevent pain by taking the tablets at a prescribed dose for up to 5-6 days before periods.
Oral Contraceptives
Some research suggests that oral contraceptives may reduce the frequency of menstrual migraines.
However, this doesn’t apply to all OCPs, and not everyone may experience the benefit.
It is also essential to discuss with your doctor any personal risk factors you may have for taking OCPs, as they can affect different women with migraine differently.
Lifestyle Changes
Much research suggests that regular exercise, especially aerobic exercise, can help prevent migraine headaches. HIIT and yoga can help too.
However, over-exertion could also be a trigger for migraines.
A regular sleep schedule, which includes clocking in 7-9 hours of daily sleep, can have magical effects on migraine in terms of reduced frequency, intensity, and duration.
Daily Magnesium
Daily oral magnesium supplement has been proven effective in preventing menstrual migraines, especially for those who experience migraine before their periods.
The mechanism behind how magnesium plays a role in preventing migraines is still hazy. Some scientists theorize that magnesium may help decrease neuronal firing.
The healthcare practitioner can decide the type and dosage of magnesium.
Please do not start any nutritional supplements without a consultation.
Relaxation Techniques
Techniques like guided meditation, breathing exercises, and yoga flow to relax muscles can help reduce stress, which is a common trigger for menstrual migraines.
Working with a healthcare provider to develop a personalized treatment plan for menstrual migraines is essential, as the best approach may vary depending on the individual.
Additionally, tracking menstrual cycles and migraine symptoms can help identify patterns and potential triggers, making it easier to prevent migraines before they occur.
Summary
A new study sheds light on the cause of menstrual migraines.
The study reports that levels of a protein called CGRP that plays a role in inflammation in the brain are higher in those experiencing menstrual migraines.
Women can make lifestyle changes, avoid triggers, use medications, consider hormonal therapy, and try alternative therapies such as acupuncture or relaxation techniques to prevent and manage menstrual migraines.
Work with a healthcare provider to develop a personalized treatment plan and track menstrual cycles and migraine symptoms to identify patterns and potential triggers.




